What is Liver Fibrosis / Cirrhosis commonly known in Singapore?
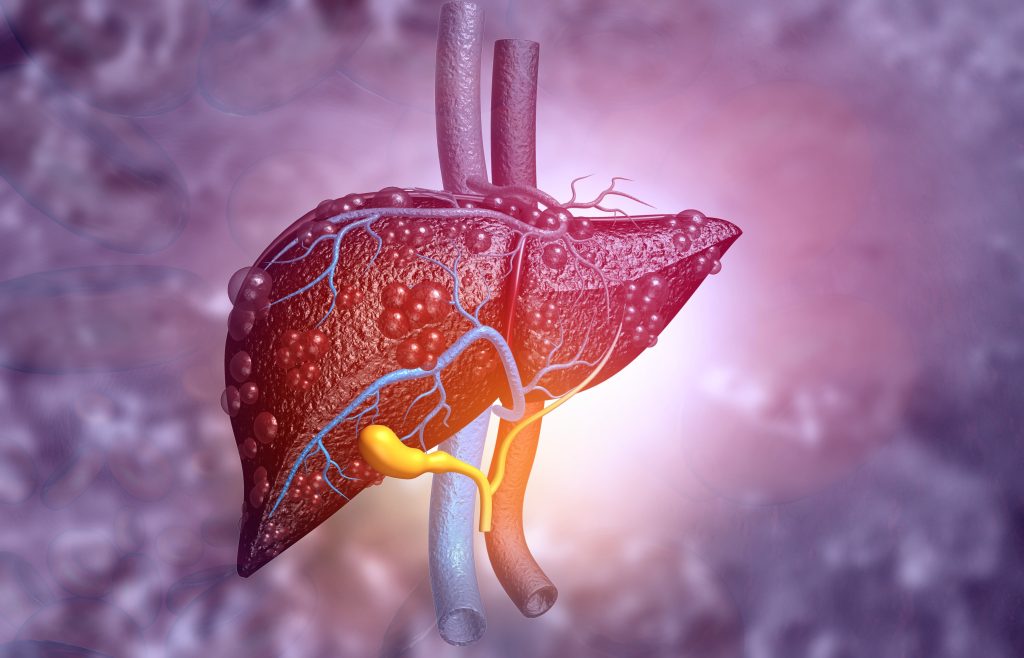
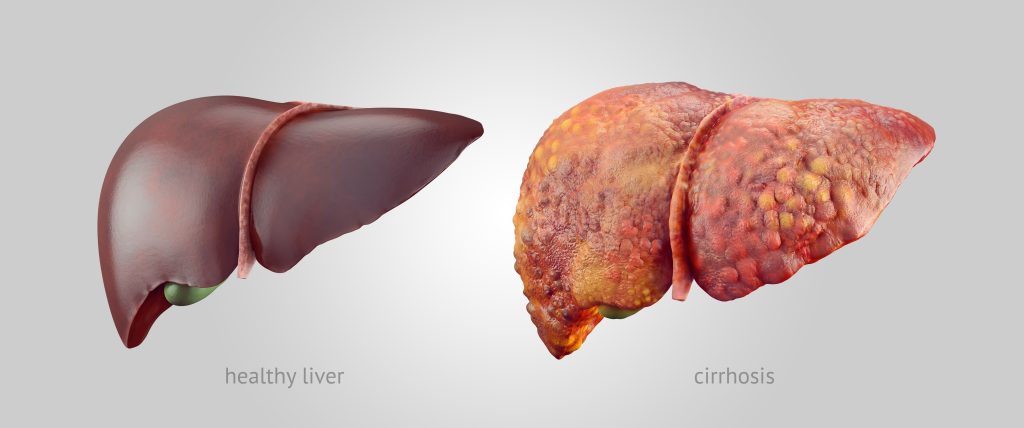
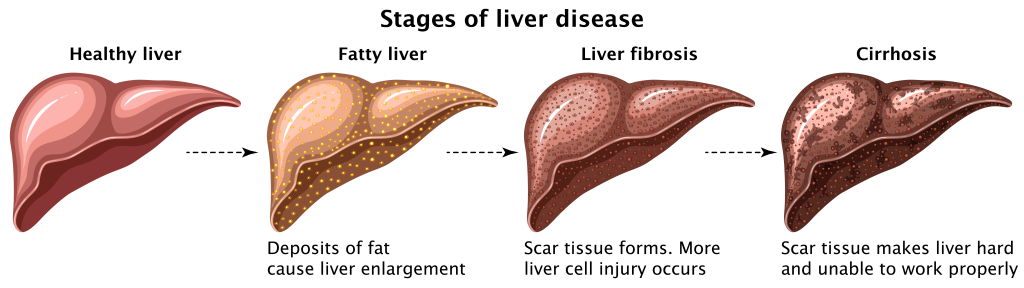
The liver is about the size of a football and rests on the upper right side of the abdomen. It is also the only organ in the human body that can heal and regenerate. However, liver cirrhosis happens as healthy liver tissue gets replaced by scar tissue in a process known as fibrosis. Scar tissue usually forms when there is an insult to the liver, i.e. there is something that injures the liver and causes its tissues to be destroyed and inflammation to take place.
Liver cirrhosis is considered a late-stage liver disease where the liver is permanently damaged. It becomes shrunken, and liver function gets impaired, affecting the organ’s ability to regenerate.
Fibrosis vs cirrhosis
Fibrosis is a medical term for scarring, and it refers to any degree of scarring in the liver. Cirrhosis, on the other hand, usually refers to a late-stage disease where scarring/fibrosis is severe and extensive.
Is fatty liver the same as Liver Fibrosis / Cirrhosis?
Fatty liver, or steatosis, is not the same as liver cirrhosis. However, it is of note that cirrhosis is caused by long-term injury to the liver, and steatosis might be a cause of liver cirrhosis if it advances and causes concurrent liver inflammation, in a process known as steatohepatitis.
Fatty liver disease is a common condition and refers to the storage of extra fat in the liver. Most people who have fatty liver disease do not have symptoms and fatty liver often does not cause serious problems. The 2 main forms of fatty liver disease are:
- alcoholic liver disease (accumulation of fat as a result of many years of heavy drinking)
- non-alcoholic fatty liver disease (NAFLD), which occurs in those who are not heavy drinkers, and are associated with conditions such as obesity and diabetes.
The stages of cirrhosis
There are 2 clinical stages of cirrhosis: 1) compensated cirrhosis and 2) decompensated cirrhosis
Compensated cirrhosis
In this phase of liver cirrhosis, patients typically do not complain of any symptoms because the remaining healthy liver cells are still able to meet the body’s metabolic needs, i.e. they are able to compensate for the damaged and scarred liver tissue and cells. Patients may feel normal and may not even know that there is liver cirrhosis.
Decompensated cirrhosis
This phase of liver cirrhosis typically causes various symptoms to arise as liver function declines. This includes that of:
- Ascites — abdominal distension as the abdominal cavity becomes full of fluid
- Hepatic encephalopathy — a loss of brain function as the body becomes unequipped to get rid of toxic chemicals that were once excreted by the liver
- Variceal bleeding — bleeding occurring from dilated blood vessels (varices) in places like the throat, small bowel, stomach - typically a medical emergency
- Jaundice — due to a build-up of bilirubin, a product produced by the liver; symptoms include yellowing of the eyes and skin, pale stools, dark-brown urine
How long does fibrosis take to cause cirrhosis?
Overall, cirrhosis is a very slow-acting disease process. While there are many causes of cirrhosis, it typically takes more than 10 years for it to develop and often, patients do not show symptoms until the late stages of decompensated cirrhosis.
What causes Liver Cirrhosis?
There are many causes of liver cirrhosis, including but not limited to:
- Chronic Hepatitis B infection (most common cause in Singapore)
- Chronic Hepatitis C infection
- Alcoholism
- NASH (non-alcoholic steatohepatitis - when there is fat in the liver as well as signs of inflammation and liver cell damage, but not due to alcohol use)
- Autoimmune liver diseases, e.g. primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC)
- Metabolic diseases, e.g. Wilson’s disease
Note that cirrhosis is not inherited and that it is also not cancer. However, cirrhosis is a risk factor for the eventual development of liver cancer and a half-yearly follow-up is important to monitor and track liver function and disease progression.
What are the symptoms of Liver Cirrhosis?

Symptoms typically only arise in decompensated or advanced cirrhosis. Symptoms of significant and severe liver damage include:
- Lethargy
- Sleep disturbances, changes in mood, confusion, agitation
- Jaundice (yellowing of eyes and skin, pale stools, dark-brown urine)
- Ascites (abdominal distension)
- Leg swelling
- Presence of red, spidery dots on the chest and back (spider naevi)
- Vomiting of fresh blood
- Passing of black, sticky stools (melena)
Dr Benjamin Yip cautions that liver fibrosis and early stage liver cirrhosis are conditions with no symptoms. However, if left untreated, it may progress to late stage liver cirrhosis where quality of life may be severely affected. Hence, it is prudent to seek the advice of a Gastroenterologist if you are found to have liver fibrosis/cirrhosis even if you feel well.
How is Liver Cirrhosis diagnosed?

First, your doctor will ask you more about your symptoms, medical history and drug history to better understand your condition. This will be followed by a physical examination to assess the liver size and whether or not there are any complications seen due to liver cirrhosis.
Blood tests may also be done. Parameters that may be assessed include but are not limited to:
- Liver function
- Checking for liver damage
- Screening for anaemia, infection
- Screening for viral hepatitis, autoimmune conditions, etc
Certain imaging tests may also be done to examine the size, shape, and texture of the liver. These imaging studies can also help to determine the amount of scarring in the liver as well as the presence of any possible fatty liver disease.
- CT scan of the liver
- MRI scan of the liver
- Ultrasound of the abdomen
- Elastography — a special ultrasound scan of the liver that can measure its fat content and how stiff the liver tissues are
- Oesophago-gastro-duodenography (OGD) to visualise the pathway from the mouth to the stomach, to check for varices and bleeding
A liver biopsy might also be done, where a sample of the liver is removed and examined under the microscope by a pathologist, who is a doctor trained in examining live tissues. Biopsies are useful for diagnosis as they help to confirm the diagnosis of cirrhosis, determine the extent of liver damage, and also assess for any cancerous changes.
How is Liver Cirrhosis treated?
The treatment for liver cirrhosis depends on the underlying cause of liver cirrhosis. Treatment for the common causes of cirrhosis are as follows:
- Alcoholic liver cirrhosis — the mainstay of treatment to delay progression is to stop drinking alcohol. Support groups /alcohol addiction treatment programmes may be an option to help patients better transition through quitting alcohol
- Hepatitis B/C — antiviral medications are the mainstay of treatment
- NAFLD (Non-alcoholic fatty liver disease) — management of comorbidities are the best way to halt progression of NAFLD and liver cirrhosis. This includes weight loss, having a healthy diet, exercising, and ensuring good compliance to any long-term medication.
Overall, the aims of treatment are to control the underlying cause of cirrhosis and to delay further progression of the disease. Long-term followup is also necessary to monitor liver function and to screen for hepatocellular carcinoma (HCC).
In advanced cases, a liver transplant may also be an option if the patient is a suitable candidate.
Can Liver Cirrhosis be cured?
Liver cirrhosis can improve and even be reversed in certain situations. Every case of liver cirrhosis is different and each patient’s prognosis will depend on multiple factors including the underlying cause of their liver cirrhosis, their current medical history, as well as how well they adhere to the medication treatments.
Overall, the main aims of treatment are to ameliorate the cause of liver injury and allow time for the liver to heal and repair itself. Early detection is key in liver cirrhosis - outcomes are the best for liver cirrhosis when treated early, as this helps to prevent further deterioration while cirrhosis is still at an early stage. When detected early and successfully managed, the progress of cirrhosis may be slowed or even stopped.
What complications can arise if Liver Cirrhosis is left untreated?
The main complications that arise from liver cirrhosis include:
- Increased risk of liver cancer — cirrhosis and scarring of the liver increases the risk of hepatocellular carcinoma (HCC), the primary type of liver cancer.
- Malnutrition — the liver processes nutrients and a damaged liver impedes the digestion and absorption of nutrients.
- Abdominal and leg swelling — fluid retention and decreased urine output commonly happen as liver function declines.
- This is because as the cirrhosis gets more advances, blood pressure in the portal vein (a blood vessel that carries blood from the intestines to the liver) gets very high, causing kidney function to worsen and fluid to build up in the abdomen
- This is because as the cirrhosis gets more advances, blood pressure in the portal vein (a blood vessel that carries blood from the intestines to the liver) gets very high, causing kidney function to worsen and fluid to build up in the abdomen
- Internal bleeding — typically due to burst varices, of which the bleeding can become life-threatening
- Hepatic encephalopathy — brain damage caused by liver failure due to the build-up of toxic chemicals that are typically excreted by the liver, This causes lethargy, confusion, changes in mood, psychosis, and can eventually lead to comas and death
How can I prevent Liver Cirrhosis?
There are several ways to prevent cirrhosis:
- Lifestyle changes
- Drinking in moderation
- Having a healthy diet with regular exercise
- Maintaining a healthy weight
- Quitting smoking
- Medical
- Ensuring good compliance to medications
- Being alert and aware of signs of jaundice, liver infection, etc
- Reducing risk factors that predispose to cirrhosis
- Avoiding risky behaviours — e.g. having safe sexual practises and not sharing needles (which reduces risk of getting hepatitis B and C respectively)
- Getting a Hepatitis B vaccination
Living with Liver Cirrhosis
Life expectancy differs between every patient and depends on several factors, including:
- Cirrhosis
- Severity of cirrhosis
- The underlying cause of liver damage
- Efficacy of medical treatment
- Patient factors
- Age
- Medical background
Summary
Liver cirrhosis is a late-stage disease and most patients are typically at an advanced stage by the time they are diagnosed. Thus, it is important to take careful watch of your health and comorbidities, and ensure that you are compliant to your medications and follow-up.
Preventive measures are also effective in helping to prevent extensive liver damage in the first place, and are good to follow in the long-run regardless of whether or not there is an aim to prevent cirrhosis, as they help to optimise long-term health and minimise the risk of any future morbidity and mortality.
References
- “Cirrhosis: Symptoms, Causes, Stages, Diagnosis, and Treatment.” WebMD, 8 December 2020, https://www.webmd.com/digestive-disorders/understanding-cirrhosis-basic-information. Accessed 30 May 2022.
- “Diagnosis of hepatocellular carcinoma - PMC.” NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2023919/#. Accessed 30 May 2022.
- Lee, Tae Hoon, and James J. Peters. “Fibrosis of the Liver - Liver and Gallbladder Disorders - MSD Manual Consumer Version.” MSD Manuals, https://www.msdmanuals.com/en-sg/home/liver-and-gallbladder-disorders/fibrosis-and-cirrhosis-of-the-liver/fibrosis-of-the-liver. Accessed 30 May 2022.
- “Liver Cirrhosis - Singapore.” NUH, https://www.nuh.com.sg/Health-Information/Diseases-Conditions/Pages/Liver-Cirrhosis.aspx. Accessed 30 May 2022.
- “Overview - - - Cirrhosis.” NHS, https://www.nhs.uk/conditions/cirrhosis/. Accessed 30 May 2022.

