Introduction
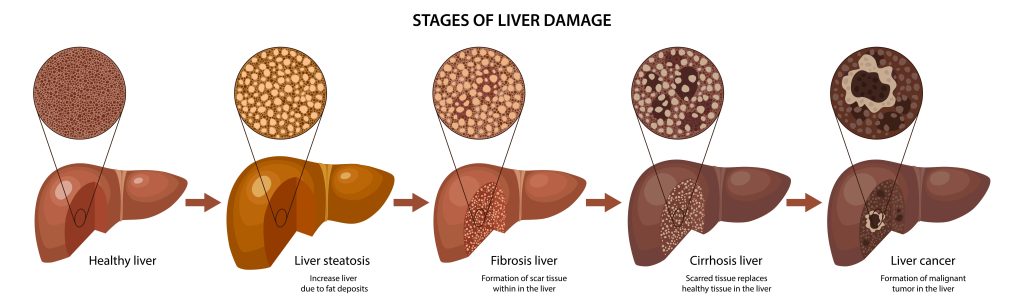
What are liver fibrosis and liver cirrhosis commonly known in Singapore? Both conditions sound similar and have similar causes — with fibrosis being the precursor to cirrhosis. Liver fibrosis arises when the liver becomes damaged and scarred, affecting its function. If left untreated and allowed to worsen over time, this scarring worsens, and the liver becomes irreversibly damaged. This is known as liver cirrhosis.
In this article, we will briefly cover the causes, symptoms and treatment of liver fibrosis and liver cirrhosis, as well as provide a detailed overview of how both conditions are assessed.
Liver fibrosis
Liver fibrosis is the result of repeated or chronic injury to the liver tissue, resulting in defective repair and the formation of scar tissue and fibrosis over time.
Broadly, liver fibrosis can be caused by any inflammation, injury, or chronic infections in the liver. Some common causes include:
- Non-alcoholic fatty liver disease (NAFLD)
- Alcoholic liver disease
- Hepatitis B and C (viral hepatitis)
- Autoimmune hepatitis
- Wilson’s disease (genetic disease causing copper overload)
- Biliary cirrhosis
Liver fibrosis is usually asymptomatic and goes undetected. Hence, it is important to screen for liver fibrosis when early liver disease is suspected.
Liver cirrhosis
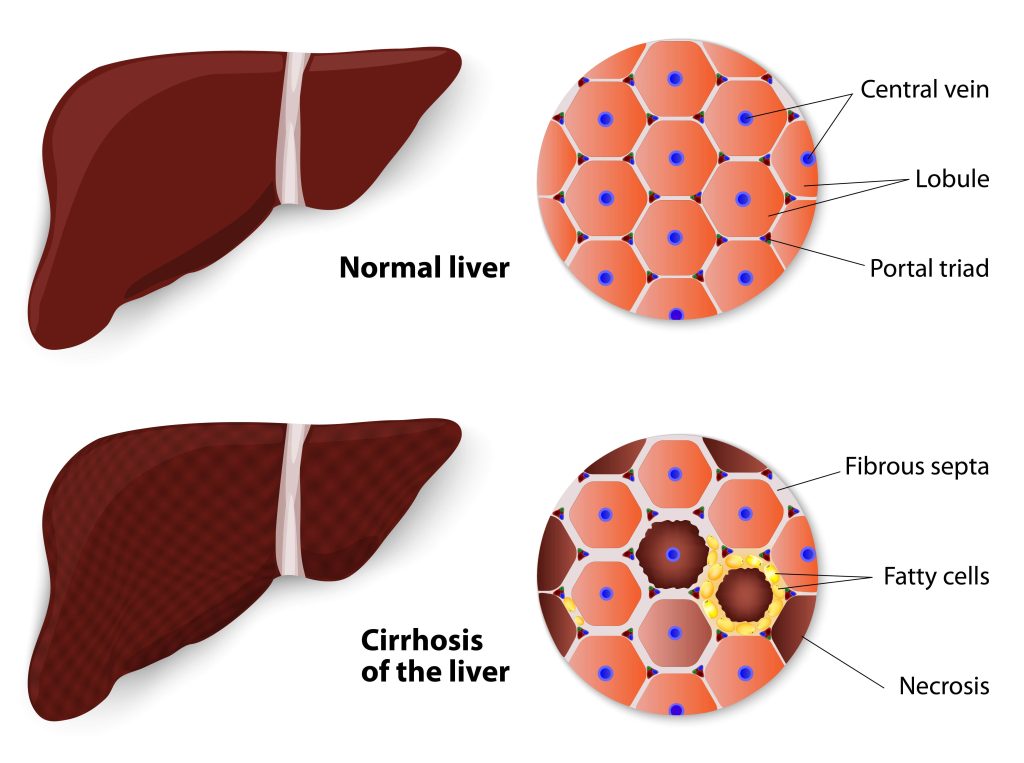
Liver cirrhosis is essentially the final stage of liver fibrosis. In fibrosis, some scar tissue is formed in the liver but does not impair the liver function as much as in cirrhosis. In liver cirrhosis, the scar tissue builds up and forms bands within the liver, affecting the physical structure/shape of the liver, irreversibly damaging the function of liver cells, and the liver is no longer able to repair itself.
Causes are largely similar to that of liver fibrosis:
- Non-alcoholic fatty liver disease (NAFLD)
- Chronic alcohol use
- Hepatitis B and C (viral hepatitis)
- Autoimmune hepatitis
- Hemochromatosis (iron overload in the body)
- Wilson’s disease (genetic disease causing copper overload)
- Biliary cirrhosis
- Medications (very rarely caused by methotrexate, isoniazid, methyldopa)
- Alpha-1 antitrypsin deficiency (genetic disorder)
Most liver cirrhosis cases in Singapore may go undetected until later stages, when significant damage has already occurred. There are many concerning symptoms associated with liver cirrhosis, including all the symptoms of liver fibrosis (mentioned above), as well as:
- Fatigue
- Easy bruising and bleeding
- Oedema (swelling of the limbs and soft tissue)
- Ascites (fluid accumulation in the tummy)
- Itchy skin (from bile buildup)
- Gynaecomastia (breast development in men)
- Testicular atrophy (in men)
- Drowsiness, confusion (hepatic encephalopathy in severe, untreated cirrhosis)
How is Fibrosis/Cirrhosis of the liver assessed?
Liver fibrosis and cirrhosis are assessed using the same modalities, to determine:
- How badly liver function is affected
- The underlying cause of the fibrosis
- The extent of damage to liver tissue
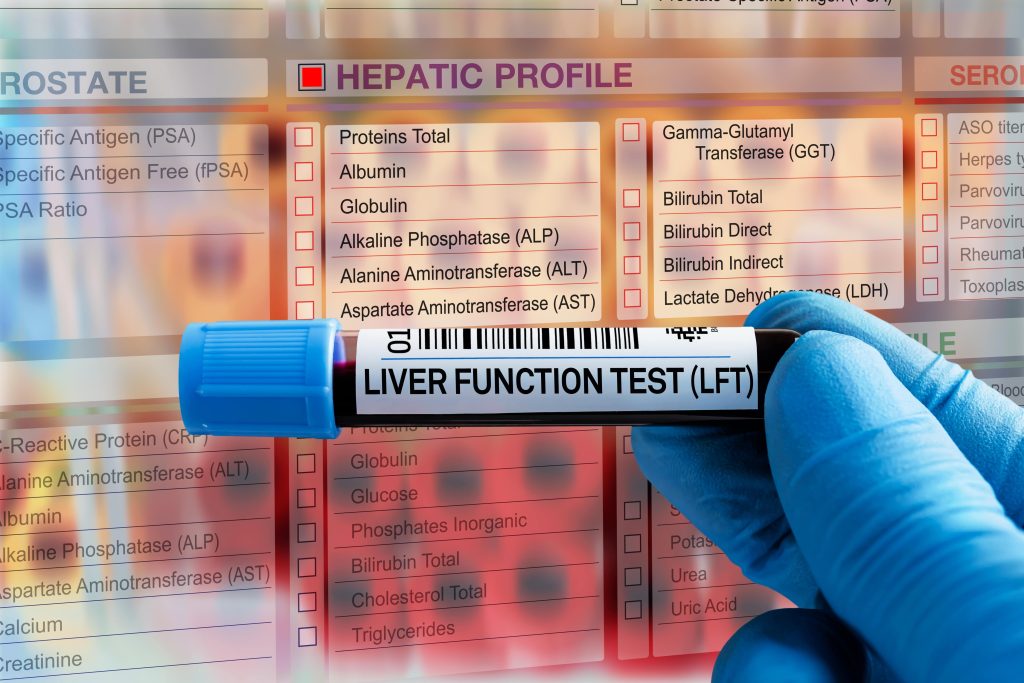
Firstly, to determine how severely the liver function has been affected, blood tests are done. To assess the liver function itself, a panel of blood tests are done: various liver enzymes (ALT, ALP, AST), bilirubin, a full blood count and PT/INR (a blood test to assess abnormal clotting).
To assess the underlying cause, further blood tests to screen for viral hepatitis B or hepatitis C will be done. If your doctor suspects an autoimmune condition (one’s own cells attacking body tissue/organs), additional tests will be done to check for the presence of: antinuclear antibodies (ANA), anti-smooth muscle antibodies (SMA), and antimitochondrial antibodies (AMA).
In cases where the cause still cannot be determined by the above blood tests, a liver biopsy (tissue sample) may be required. It is done under ultrasound guidance, so the doctor is able to visualise the insertion of the needle at the site of intended biopsy. The tissue sample will be tested further to ascertain the cause of liver fibrosis.
The extent of damage can be assessed by non-invasive imaging tests such as Magnetic Resonance Elastography (MRE). Combining MRI techniques with vibrations directed at specific sites, an image called an elastogram is generated, allowing the doctor to assess the areas of fibrosis (stiffening) or cirrhosis (hardening).
The MRE scan is often done during an MRI of the liver, with an additional elastography component. An MRI involves lying down on a table which moves you into an enclosed tunnel; the duration of an MRI scan is approximately 30-45 minutes.
An alternative to MRE, Transient Elastography (TE) or FibroScan, can also be used to quantify liver fibrosis and measure liver stiffness. This non-invasive diagnostic test utilises ultrasound and low-frequency elastic waves directed into the liver.
From your fibrosis score, results generally range from normal i.e. no scarring to advanced i.e. frank liver cirrhosis:
- Normal — no scarring or mild scarring of the liver.
- Moderate to severe — liver scarring that may be reversed or slowed down.
- Advanced — this refers to cirrhosis, the most advanced form of liver scarring.
What are my treatment options for liver fibrosis/cirrhosis?
The treatment options for both conditions involve treating the underlying cause and preventing further progression or damage to the liver tissue. If the patient has significant symptoms, treatment is targeted at managing symptoms as well.
Treatment of the underlying cause:
- Non-alcoholic fatty liver disease (NAFLD) - losing ~10% of one’s body weight improves the disease and reduces the risk of cirrhosis
- Chronic alcohol use - alcohol cessation programmes and counselling
- Hepatitis B and C (viral hepatitis) - antiviral medication to control any active hepatitis
- Autoimmune liver diseases - medications (steroids, other immunosuppressive agents) to control the disease
Not all of the causes of liver fibrosis/cirrhosis have treatments available, hence managing symptoms would be important as well.
For symptomatic management, medications to reduce itch, pain, and fatigue are available, as well as supplements to replace any deficient minerals, as cirrhosis is associated with osteoporosis and malnutrition.
For patients with oedema (swelling of the limbs and soft tissue) and ascites (fluid accumulation in the tummy), a low salt diet, combined with a restriction on the amount of fluids one can consume, will help relieve the swelling. If the ascites becomes significant and affects one’s daily function, a small catheter may need to be inserted to drain the fluid. If an infection of the ascitic fluid occurs, one may require antibiotics and hospitalisation.
Due to the hardened structure of a fibrotic/cirrhotic liver, there is increased blood pressure, termed portal hypertension. Blood pressure lowering medications help to reduce the pressure in the liver vessels and reduce the chances of severe bleeding. If portal hypertension is poorly controlled, one may develop oesophageal or gastric (stomach) varices, which are enlarged veins with a high risk of bleeding. Regular endoscopy may be required, with surgery if the veins bleed.
Unfortunately, liver cirrhosis confers an increased risk of liver cancer (hepatocellular carcinoma, HCC). Regular follow-up visits, blood tests and ultrasound exams will be done as surveillance.
In advanced liver cirrhosis, when the liver is no longer able to function, a liver transplant may be performed. The liver may be obtained from a cadaver (deceased donor) or living donor.
Summary
In summary, liver fibrosis and liver cirrhosis are progressive diseases of the liver with various underlying causes. While the injury and damage to the liver may not be reversible, there are various ways to slow down the progression of liver fibrosis into liver cirrhosis.
We hope this article has been useful in educating you about the causes, symptoms, assessment and treatment of liver fibrosis and liver cirrhosis. If you have any further queries, do seek a consultation with a medical professional.
References
- Diagnosing Liver Fibrosis: Choosing the Right Test for You. (2020, March 26). UVA Radiology and Medical Imaging Blog for Patients. Retrieved April 22, 2022, from https://blog.radiology.virginia.edu/diagnosing-liver-fibrosis/
- Lee, Tae Hoon, and James J. Peters. “Cirrhosis of the Liver - Liver and Gallbladder Disorders - MSD Manual Consumer Version.” MSD Manuals, https://www.msdmanuals.com/home/liver-and-gallbladder-disorders/fibrosis-and-cirrhosis-of-the-liver/cirrhosis-of-the-liver. Accessed 20 September 2022.
- “Diagnosis of Cirrhosis | NIDDK.” National Institute of Diabetes and Digestive and Kidney Diseases, https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis/diagnosis. Accessed 20 September 2022.
- “Ultrasound-Guided Liver Biopsy.” Cedars-Sinai, https://www.cedars-sinai.org/programs/imaging-center/exams/ultrasound/liver-biopsy.html. Accessed 20 September 2022.
- Bhan, Irun. “Weight loss can help head off lasting damage caused by fatty liver.” Harvard Health, 30 April 2020, https://www.health.harvard.edu/blog/weight-loss-can-help-head-off-lasting-damage-caused-by-fatty-liver-2020043019664. Accessed 20 September 2022.

