
What is an EUS?
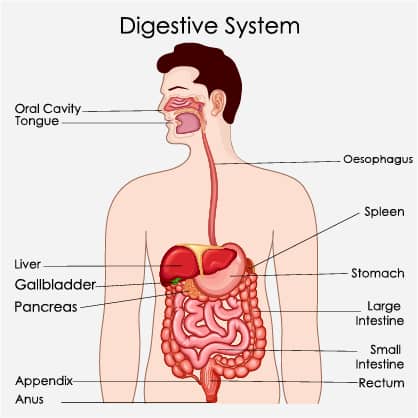
An Endoscopic Ultrasound (EUS) is a minimally invasive procedure used to assess the digestive tract, including the lining of your upper (oesophagus, stomach and duodenum) and lower (colon and rectum) gastrointestinal tract. It also allows the gastroenterologist to examine structures adjacent to the GI tract, such as the pancreas, liver, gallbladder and bile duct as well as lymph nodes, tumours, and fluid collections.
During this procedure, the gastroenterologist will insert a flexible, hollow tube called an endoscope either through your mouth or rectum (Rectal Endoscopic Ultrasound) and down into your digestive tract. Patients are typically given sedation so they do not feel any pain during the procedure.
The endoscope used in an EUS is equipped with a video camera and an ultrasound scanning probe at its end. The video camera allows doctors to have a direct image of your digestive tract, while the ultrasound probe uses high-frequency sound waves to produce detailed images of the linings of your digestive tract, as well as nearby organs. Because an Endoscopic Ultrasound is performed inside the body, the ultrasound waves can penetrate deeper than an ultrasound examination conducted from the body’s surface.
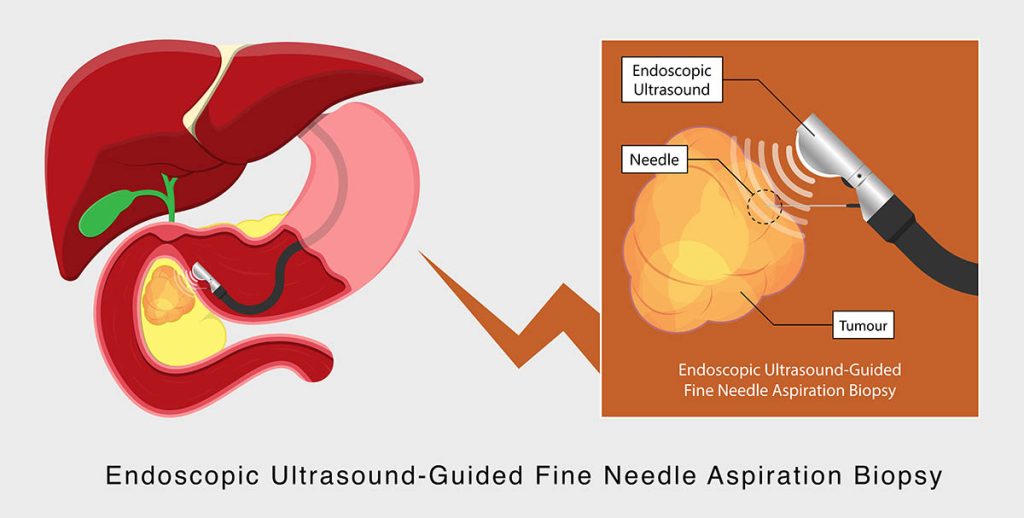
Endoscopic Ultrasound-Guided Fine Needle Aspiration (EUS-FNA) Biopsy
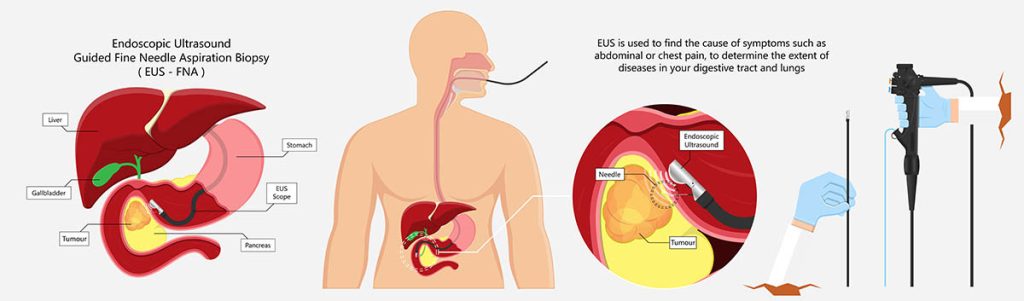
During the EUS, another procedure called a fine-needle aspiration (FNA) might also be performed. FNA involves the use of a small, thin needle, and it is used to remove small tissue samples (biopsy) from your abdomen for analysis.
Once the EUS procedure is over, the FNA sample will be sent to a laboratory. The sample will then be analysed by a pathologist – a medical professional who has specialised in interpreting and evaluating the human body and its tissues. Any abnormalities that are detected in the sample will be included in the pathology report so that your gastroenterologist can refer to it and discuss the diagnosis with you. The report is also beneficial to discern any further steps that need to be taken with regard to your treatment plan.
Overall, in comparison to exploratory abdominal surgery, an Endoscopic Ultrasound that is carried out in conjunction with an FNA is an ideal alternative option as it is minimally invasive.
While the EUS procedure is generally safe and has minimal side effects, there may still be some risks involved, such as:
- Pain
- Bleeding
- Infection
- Adverse reactions to sedation administered
- Injury to nearby structures and organs
- Bowel perforation
- Pancreatitis (if an FNA of the pancreas is done)
When would I need an EUS?
Endoscopic ultrasounds are used to address and treat a wide range of abdominal conditions – the indication for an EUS can be both diagnostic and therapeutic.
Diagnostic purposes
An Endoscopic Ultrasound is beneficial in assessing both upper and lower gastrointestinal tract conditions, including:
- Bile duct stones
- Pancreatic cysts
- Any form of cancer in the digestive tract (oesophagus, stomach, rectum, pancreas)
- Any abnormal growths in the digestive tract (stomach, oesophagus, rectum)
- Lymphoma and enlarged lymph nodes in the abdomen and chest
During your endoscopy procedure in Singapore, a tissue sample may also be obtained by a fine needle biopsy (FNA) for more detailed analysis in order to confirm the diagnosis.
Therapeutic purposes
An Endoscopic Ultrasound has the benefit of treating certain medical conditions without the need for incisions or surgery. Some of these therapeutic treatments include:
- Drainage of pancreatic cysts
- Aspiration of fluid-filled spaces in the abdomen
- Treating any bleeding in the digestive tract from a burst blood vessel
- The treatment of pancreatic diseases by applying nerve blocks
- Various ablative therapies
Why is an EUS important?
Endoscopic Ultrasound plays an integral role in the assessment and evaluation of gastrointestinal diseases and anomalies as they are safe (minimally invasive), effective and have a high sensitivity in detecting certain anomalies in comparison to other investigations.
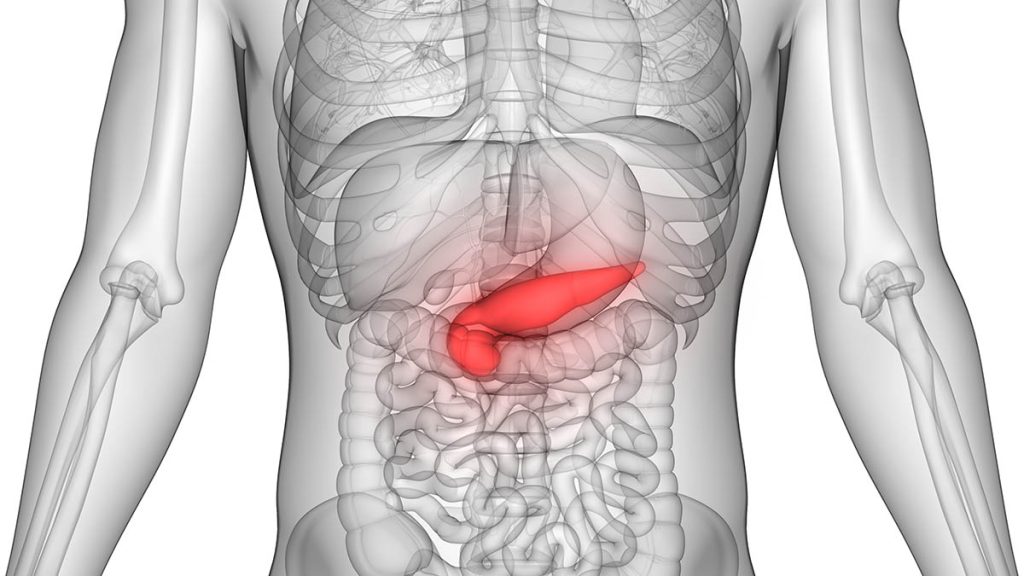
In Dr Benjamin Yip’s personal opinion, the EUS is a procedure tailor-made for the pancreas, which is a deep-seated abdominal organ. It is located behind the stomach in the upper left abdomen and is surrounded by many organs and structures, such as the small intestine, liver and spleen.
Due to the configuration of the stomach and duodenum, an EUS can be conveniently used to access the pancreas in a minimally invasive manner, either for diagnostic or therapeutic requirements. If not, the pancreas would generally need to be accessed percutaneously (through the skin), which would often not be possible due to the location of the pancreas.
How do I prepare for an EUS?
Before your endoscopy in Singapore, you will be given certain specific instructions to help yourself prepare for the procedure. It is important to follow these instructions carefully.
In general, these instructions will include the following:
- Fasting before EUS – Patients are usually required to fast ≥ six hours before their Endoscopic Ultrasound in Singapore.
- Bowel preparation (if the EUS is done in the rectal area) – You may be asked to take a laxative or enema beforehand and to follow a liquid diet a day or two before the procedure. This will help to clear the bowel before the procedure so that a clear, clean and detailed view can be obtained.
- To stop taking certain medications – These include anticoagulants (blood thinners), which can increase the risk of bleeding during your EUS procedure, especially if an FNA is being performed. Your doctor will go over your medication regime in further detail with you in the days leading up to the EUS because it is very patient-specific.
- Plan ahead before your discharge – Make arrangements to have someone accompany you home after the procedure. As sedation is used in Endoscopic Ultrasounds to help the patients relax and minimise discomfort, you should refrain from driving immediately after discharge as the effects of sedation tend to last for several hours post-EUS. In addition, you are entitled to take one or two days of medical leave to recuperate completely.
What can I expect during my EUS procedure?

Regardless of the indications for the procedure, the process of the EUS remains largely the same. It is performed as a day procedure, and patients can typically go home on the same day, around two hours following the procedure.
Prior to the procedure, sedation will be administered to block any pain or discomfort during the procedure. It is usually safe and will help you fall asleep. As the EUS is performed inside your digestive tract, there will be no injury to the skin.
Once sedated, the EUS endoscope will be passed through your mouth or rectum, and the doctor will then observe the insides of your digestive tract through a standard monitor and an ultrasound monitor by the bedside.
If an FNA is required, a small thin needle will be inserted through the EUS endoscope, which will emerge from its tip – Endoscopic Ultrasound-Guided Fine Needle Aspiration. As mentioned previously, small tissue samples will then be removed from your gut lining and will be sent to a laboratory for a pathologist to examine.
At the end of the procedure, the endoscope will be withdrawn from the body, and you will be woken up shortly after that. Overall, the entire EUS procedure tends to take around 60 minutes to complete.
Is the EUS a painful procedure?
As you will be put under sedation, you generally will not be expected to feel any pain. However, you may feel slight discomfort when you first swallow the endoscope. If general anaesthesia (GA) is administered, you will be asleep throughout the entire procedure.
Post-EUS
Aftercare
After the EUS procedure, you will be taken to a recovery room where you can rest and slowly wake up from the sedation. During this period, your vital signs will be continuously monitored, and adequate care will be rendered to you.
Your doctor or primary care team might also come to check up on you and explain any findings found during the EUS-FNA procedure.
Recovery time usually takes around one hour: Once you have recuperated, you will be discharged with certain medications and important care instructions. Additionally, your follow-up care plans will be discussed. Having performed countless Endoscopic Ultrasounds in Singapore, Dr Benjamin Yip understands the risks of driving and operating machinery after sedation. Therefore, his advice is to arrange for someone you trust to accompany you home during this period, as you should refrain from carrying out such activities.
What can I eat or drink after my EUS procedure?
- Generally, you are allowed to resume your usual diet two hours after the procedure. You’re also encouraged to avoid alcohol at least 24 hours after your procedure.
- If you experience a slight sore throat post-procedure, you can take warm liquids, throat lozenges or prescribed painkillers to ease the discomfort.
Are there any contraindications for the EUS procedure?
While most patients can undergo an Endoscopic Ultrasound, there might be a few instances in which this procedure may be contraindicated. These instances include:
- If there is difficulty with visualising the lesion
- In cases with bleeding diathesis (bleeding susceptibility)
- Tumour seeding (dislodging and spread of malignant cells due to the needle – rare)
- If the tumour or a vessel is located in between the FNA needle and the targeted site
Side effects and complications
If an FNA is performed during the EUS, you might feel some slight soreness in your abdomen, but this will usually resolve within one to two days. Overall, EUS is a fairly safe procedure, and side effects should be minimal. You can reduce the risk of complications by carefully following the instructions given to you by your medical care teams.
Some warning signs to look out for include:
- Severe and persistent abdominal pain
- Black stools or bloody stools
- Fever
- Chest pain
Should you experience any of the above symptoms, please seek medical attention immediately.
Summary
Overall, an Endoscopic Ultrasound is a minimally invasive and safe procedure that allows for both diagnostic testing and therapeutic treatment for various abdominal conditions. It is a safe alternative to surgery and facilitates a range of comprehensive medical care and treatment.
Dr Benjamin Yip believes that interventional EUS is one of the quickest moving areas in advanced endoscopy — “With the advent of various lumen apposing metal stents (LAMS), novel minimally invasive procedures are being added to the repertoire of the advanced endoscopist. Many of these procedures can only be achieved with surgery in the past!”
References
- ASGE | Endoscopic Ultrasound (EUS), Fine Needle Aspiration (FNA), https://www.asge.org/home/about-asge/newsroom/media-backgrounders-detail/endoscopic-ultrasound-(eus)-and-fine-needle-aspiration-(fna). Accessed 7 May 2022.
- "Durability and long-term outcomes of direct EUS-guided gastroenterostomy using lumen-apposing metal stents for gastric outlet obstruction."PubMed, https://pubmed.ncbi.nlm.nih.gov/30705945/. Accessed 7 May 2022.
- “Endoscopic ultrasound.” Mayo Clinic, 29 May 2020, https://www.mayoclinic.org/tests-procedures/endoscopic-ultrasound/about/pac-20385171. Accessed 7 May 2022.
- “Endoscopic Ultrasound (EUS) | Johns Hopkins Division of Gastroenterology and Hepatology.” Johns Hopkins Medicine, https://www.hopkinsmedicine.org/gastroenterology_hepatology/clinical_services/advanced_endoscopy/endoscopic_ultrasound.html. Accessed 7 May 2022.
- McAlpin, John. What Can I Eat After an GI Upper Endoscopy (EGD)?, 14 March 2019, https://www.dhcoftx.com/blog/what-can-i-eat-after-an-upper-endoscopy-egd/. Accessed 7 May 2022.
“Pancreas: What Is It, Function & Location.” Cleveland Clinic, 25 August 2021, https://my.clevelandclinic.org/health/body/21743-pancreas. Accessed 7 May 2022. - The Leeds Teaching Hospitals. “Endoscopic Ultrasound”, NHS. Accessed 1 August 2023. https://www.leedsth.nhs.uk/a-z-of-services/endoscopy/about-your-procedure/therapeutic-endoscopy-and-colonoscopy/endoscopic-ultrasound/
- Journal of Gastroenterology and Hepatology. “Interventional Endoscopic Ultrasonography”, Medscape. Accessed 2 August 2023. https://www.medscape.com/viewarticle/707615_3

