What are Tumour Markers?
A tumour refers to a growth in the body that results from uncontrolled cell division and can occur due to a myriad of reasons, including genetic mutations, environmental exposure, or as a result of ageing. A tumour may either be benign (non-cancerous) or malignant (cancerous). Malignant tumours tend to be more aggressive and have the potential to spread to other parts of the body.
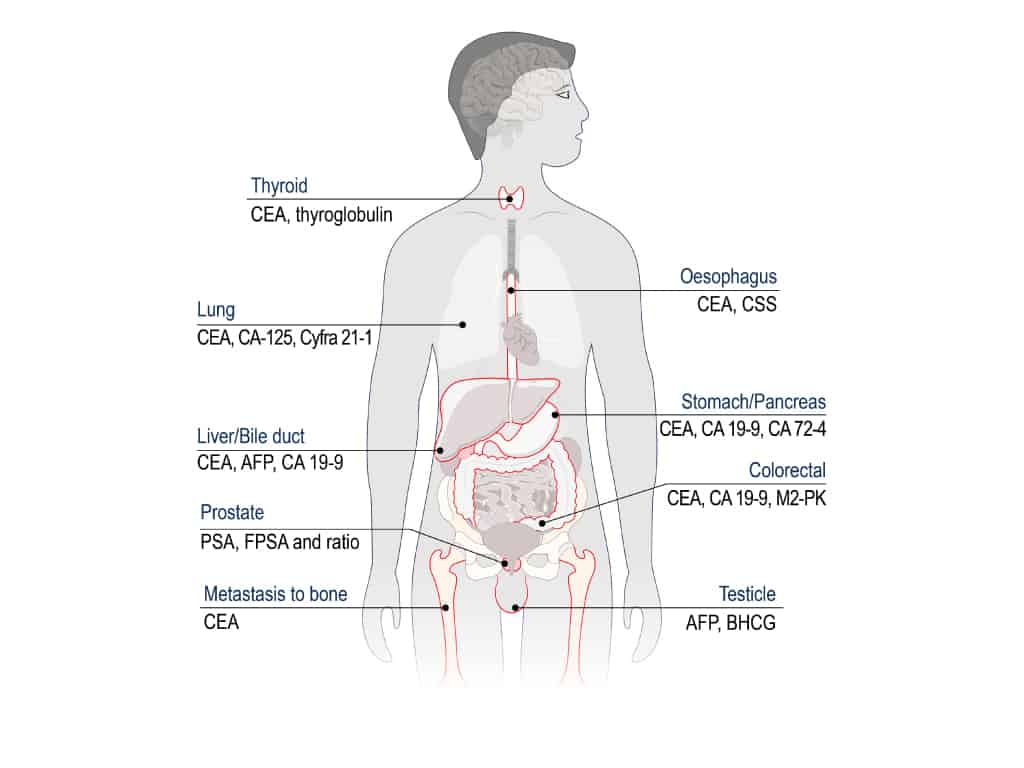
Tumour markers refer to substances produced in large quantities by cancer cells or in other cells in the body in response to the presence of a tumour. Tumour markers can provide information about a cancer, including how aggressive it is and whether it can be treated with certain targeted therapies. They can also be used during the treatment process to track the response to treatment.
Broadly speaking, common digestive tumour markers (gastrointestinal, liver, biliary tract and pancreatic cancers) include alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA) and CA 19-9).
Dr Benjamin Yip explains: “Tumour markers tests are commonly performed as part of a health screening package. They can provide useful information for the diagnosis of cancer and other medical conditions”. If a high level of digestive tumour marker is found, it is imperative that you consult a Gastroenterologist (a medical doctor who specialises in conditions concerning your digestive system) to discuss the next steps in your treatment plan.
Carcinoembryonic Antigen (CEA)
CEA is a type of oncofetal antigen, which is a substance produced by tumours and foetal tissues, with much lower concentrations present in normal adult tissues such as the intestines, pancreas, and liver.
In general, mild to moderate elevations in CEA are found in those with benign diseases in the colon, pancreas, liver and lungs. These may range from diseases such as liver cirrhosis, hepatitis, pancreatitis, inflammatory bowel disease, bronchitis, and pneumonia to certain autoimmune diseases. When the levels of CEA are markedly elevated and rise continuously in an exponential fashion, this may imply the presence of malignant cancers of the colon as well as metastatic cancers that might have spread to the bone, liver, lung and lymph nodes.
In clinical practice, CEA is used primarily to track the response to treatment in those with colorectal cancer, and it is used to monitor for cancer remission as well as any potential relapse (when the CEA levels rise again after recovery) following surgery.
In the general population, however, CEA is neither sensitive nor specific to be used as a general screening test for colorectal cancer. It would be more prudent to follow national guidelines such as doing a yearly faecal blood test for screening, e.g., a faecal immunochemical test (FIT) or faecal occult blood testing (FOBT). In addition, if you are 50 or older, it would be advisable to undergo a colonoscopy every five to ten years.
Alpha Fetoprotein (AFP)
AFP is a glycoprotein that is formed in the foetus (a developing baby inside the mother's womb during pregnancy). It is present in the yolk sac of the foetal embryo, as well as in the liver and gastrointestinal tract of the foetus. It can be detected during the 4th week of pregnancy onwards, and its level peaks around weeks 12-15 before falling continuously until birth. By the age of 1, AFP levels in the body stabilise and stay at the same low concentration until adulthood.
AFP is useful for obstetrics as it can help to detect any foetal abnormalities and diseases in the foetus. In adults, AFP may be raised in those with benign liver diseases such as hepatitis and other conditions like primary liver cancer (hepatocellular carcinoma or HCC) and germ cell tumours. Furthermore, raised AFP levels may also be found in certain patients with metastatic breast, lung, and colorectal cancers that have spread to the liver.
In clinical practice, AFP is useful in helping to monitor treatment progress for HCC and is usually done in conjunction with other tests to help diagnose HCC in high-risk groups, such as those with chronic Hepatitis B infection, where a liver ultrasound and AFP blood test are performed every six months to check for the development of HCC.
Carbohydrate Antigen 19-9 (CA 19-9)
CA19-9 is a glycolipid found in foetuses that is produced in the lining or epithelium of the stomach, intestine, and pancreas. In adults, CA19-9 exists in very low levels in the pancreas, liver and lungs, as well as in many mucosal cells.
Because it is eliminated by bile, CA19-9 levels may be raised in cases where there is bile duct obstruction, as bile cannot get released, leading to CA19-9 levels building up in the body. CA19-9 may also be raised in cystic fibrosis (a genetic condition) and inflammatory bowel disease.
In terms of cancer management, CA19-9 is the cancer marker of choice for pancreatic cancers. High levels >1000U/ml suggest lymph node spread, and levels >10,000U/ml may indicate that the pancreatic cancer has spread to other parts of the body. CA19-9 is also associated with stomach cancer, although it is less sensitive and specific and is not used as a screening.
What are Digestive Tumour Markers for?
The usefulness of clinical tumour markers and their use as a general screening tool is still under debate, although they may play a role in follow-ups of cancer treatment and to help detect relapse or further spread of cancer. For example, current-day research states that CEA is typically used for colon cancer follow-up, AFP for HCC detection and management, and CA19-9 for pancreatic cancer.
While there are many different tumour markers for different kinds of cancer, not all markers are specific for just one type of cancer and tumour markers may not necessarily always indicate the presence of cancer and may be associated with other non-cancerous health conditions as well.
Who needs to undergo Digestive Tumour Marker tests?
Patients who fulfill one or more of the following conditions might benefit from doing digestive tumour marker tests:
- Symptoms related to the digestive system: Individuals experiencing symptoms related to the digestive system, such as unexplained weight loss, abdominal pain, changes in bowel habits, or bloody stool, may undergo digestive tumour marker tests to help identify potential issues.
- Family history of digestive cancers: People with a history of digestive system cancers, such as colorectal cancer, may be monitored with tumour marker tests for surveillance and early detection of recurrence.
- Monitoring Treatment Response: Individuals undergoing treatment for digestive system cancers may have tumour marker tests to monitor the response to therapy and assess the effectiveness of the treatment.
What does it mean to have raised Digestive Tumour Markers?
Raised tumour markers may indicate a number of factors, including the formation of cancer in the body, cancer recurrence, and other medical issues. However, it is important to note that raised cancer markers alone are not a firm indicator for any diagnosis, and other tests have to be conducted for a definitive diagnosis. This includes taking a thorough medical history, physical examination, blood tests, imaging studies including X-rays and CT scans, as well as tissue biopsies.
Cancer markers, when used as part of follow-up and monitoring during ongoing cancer treatment, can be useful in signifying either a cancer recurrence or that treatment is ineffective. This may signal to your doctor that there may be a need to use stronger medication, a different drug, or a different kind of treatment altogether.
Can stress cause Digestive Tumour Markers to rise?
Currently, there is no conclusive research finding to depict an association between psychological stress and digestive tumour markers. However, certain benign, non-cancerous medical conditions may cause certain tumour markers to rise, such as CEA in pancreatitis, although these elevations often tend to be transient and will resolve once the condition is cured.
What does it mean when tumour marker levels go down?
Tumour marker levels may fluctuate over the course of the treatment, but if tumour marker levels decrease, it could imply that the treatment is working. However, this cannot be determined by these tests alone and would be required to be performed in conjunction with other diagnostic tests.
What are the tests for Digestive Tumour Markers AFP, CEA and CA 19-9?
Tumour markers are tested by blood tests. Samples will be sent to a lab for testing, and the results will then be interpreted by your Gastroenterologist.
How are tumour marker tests carried out?
There are a number of ways in which a tumour marker test is performed. They are most commonly done by taking a blood test, but a biopsy or a urine test may also be used to check for tumour markers. While you will not need any special preparations for your blood or urine test, you may be asked to fast several hours before a biopsy.
How will the tumour marker tests be interpreted?
If the report shows a high level of tumour markers, it may hint towards the presence of cancer, but this alone is not sufficient to confirm the diagnosis, and further testing will be required to find the cause of the high levels. You may also be asked to repeat the tumour marker tests in some cases, as these levels may change over time.
In some instances, tumour marker tests may also show a “false positive” or “false negative” result, which would warrant further assessments. A “false positive” indicates the individual has cancer even if it is not the case, and a “false negative” would suggest the patient does not have cancer when he or she actually does.
Are there any limitations for tumour marker tests?
Yes. While cancer marker tests do provide valuable information, they may have some limitations, including the following:
- Certain tumour markers are non-specific and can be raised by a variety of malignancies or illnesses.
- Tumour marker tests may produce "false positive" or "false negative" results.
- Some cancers may not have any known tumour markers, and some patients may not have high tumour marker levels despite having a condition like cancer that usually produces cancer markers.
- Tumour marker levels can fluctuate, making it challenging to get consistent measurements.
- Levels may not rise until the condition has reached an advanced stage.
Are there any risks to performing a tumour marker test?
No, not necessarily. Tumour marker blood tests and tumour marker urine tests usually do not have any risks, but some patients may experience mild discomfort following a biopsy. However, there is no cause for concern as these side effects typically dissipate within a short time.
Summary
When interpreted appropriately, tumour markers may be useful in helping detect your risk for certain conditions and in helping track the efficacy of treatment. Tumour markers must be used and interpreted carefully while taking into account patients’ symptoms, clinical signs, and the results of other investigations done during the care process.
Visit Alpha Digestive & Liver Centre
If you are experiencing symptoms related to the digestive system, such as unexplained weight loss, abdominal pain, changes in bowel habits, bloody stool, or have a family history of gastrointestinal cancers, you can book a screening appointment with our Gastroenterologist Dr Benjamin Yip.
References
- Mayer, RJ. “The use of serologic tumor markers in gastrointestinal malignancies.” PubMed, https://pubmed.ncbi.nlm.nih.gov/8707771/. Accessed 16 November 2022.
- “Tumor Markers in Common Use - NCI.” National Cancer Institute, 11 May 2021, https://www.cancer.gov/about-cancer/diagnosis-staging/diagnosis/tumor-markers-list. Accessed 16 November 2022.
- “Tumour Marker Tests”, Cancer.Net. https://www.cancer.net/navigating-cancer-care/diagnosing-cancer/tests-and-procedures/tumor-marker-tests Accessed 21 November 2023.
- “Tumour Markers”, Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/24813-tumor-markers Accessed 18 December 2023.
- “Tumour Markers”, Canadian Cancer Society. https://cancer.ca/en/treatments/tests-and-procedures/tumour-markers Accessed 18 December 2023.

