What is GERD commonly known in Singapore?

Gastroesophageal reflux disease, or GERD, is a common condition in Singapore where acidic content in your stomach frequently flows up into your oesophagus, a muscular tube that connects your mouth to the stomach. This acid regurgitation or backwash results in a “burning sensation” behind the chest wall that we often refer to as heartburn.
What is the difference between Heartburn, Acid Reflux and GERD?

Acid Reflux
Acid reflux occurs when acidic contents of the stomach flow back into the oesophagus, causing symptoms like heartburn, abdominal pain (especially after meals), and a bad taste in the mouth.
GERD
When acid reflux is chronic and more severe, this will be classified as a medical condition, GERD. It can significantly affect the quality of your life as it comes with the risk of tissue damage and scar tissue formation.
Heartburn
Heartburn is a symptom, not a condition in itself. Although the term implies it originates from the heart, this symptom actually arises from the oesophagus.
What are the common causes of GERD in Singapore?
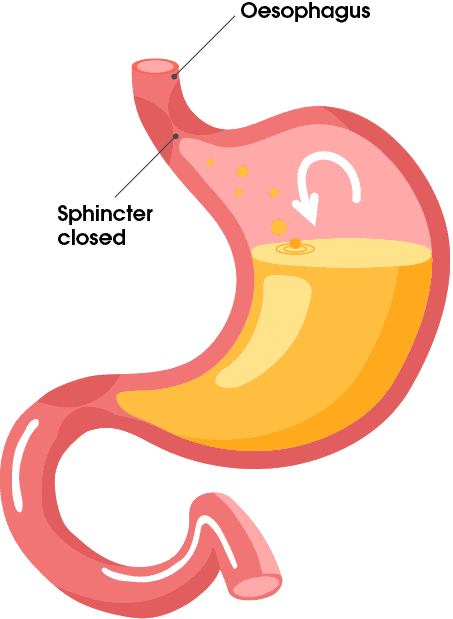
Healthy Stomach
GERD
Acid goes up into your oesophagus when the Lower Oesophageal Sphincter (LOS) relaxes abnormally or weakens. The LOS regulates the flow of food content from the oesophagus into the stomach and prevents stomach acid from being pushed back into the oesophagus.
GERD can occur as a result of stomach acid flowing frequently back into the oesophagus.
Those at a higher risk of developing GERD:

Obese – carrying extra weight can increase intra-abdominal pressure, reduce LOS pressure, and impair gastric emptying.

Pregnant – hormonal changes may decrease the LOS pressure and affect the muscles of the digestive tract, increasing the risk of heartburn and GERD.

Have a hiatal hernia – when the top of your stomach bulges through the muscle separating your abdomen and chest.

Have a connective tissue disorder – as the LOS consists of connective tissues, oesophageal function might be affected.
Behaviours or habits which increase the risk of developing GERD include:

Smoking

Eating large meals or eating late at night

Eating fatty, spicy or fried foods often

Drinking carbonated or acidic beverages often

Frequently taking certain medications such as progesterone, sedatives, or narcotics
These underlying conditions and behaviours can cause the diaphragm to weaken or become less intact, compromising the ability of the LOS to prevent acid reflux.
Eating large meals, in particular, causes the upper stomach to distend or over-stretch, causing a reduction in LOS pressure, which impairs the sphincter’s ability to prevent acid reflux.
Common symptoms of GERD in Singapore

The stages of GERD are determined by the severity of acid reflux and can be classified into four stages:
Stage 1: Mild GERD
A little acid reflux occurs once or twice a month, which may happen together with heartburn. Heartburn will feel like a burning pain behind the breastbone in the chest.
The pain is usually tolerable and can be easily managed with painkillers. Over-the-counter acid reflux medication and lifestyle changes will be enough to ease symptoms.
Stage 2: Moderate GERD
Acid reflux and heartburn occur a lot more frequently, with increasing intensity. The pain can affect daily activities, and patients will need to be prescribed daily acid reflux medication as over-the-counter medication may not work anymore.
Stage 3: Severe GERD
The symptoms are painful and do not ease even with medication. Such symptoms include heartburn, chest pain, problems swallowing, regurgitation of food or stomach acid, persistent dry cough, and the frequent feeling of a lump in the throat.
Quality of life is severely worsened, and your gastroenterologist may recommend surgery to treat your GERD in Singapore.
Stage 4: Precancerous lesions or Cancer
Repeated damage from years of severe untreated acid reflux may lead patients to develop a precancerous condition known as Barrett’s oesophagus. If left untreated, it may progress to cancer.
What is Barrett’s Oesophagus?
Barrett’s oesophagus is a premalignant condition in which oesophageal cells mutate into cells resembling those in the intestine, predisposing to the development of oesophageal adenocarcinoma, a rare cancer.
This condition may develop as a severe complication of GERD, where the oesophagus becomes damaged (thickens and reddens) as a result of chronic exposure to stomach acid.
Many patients with Barrett’s oesophagus do not have any symptoms. But those who develop the condition due to long-standing GERD may experience the following symptoms:
- Painful swallowing
- Chronic sore throat
- Sour taste in the mouth
- Bad breath
- Unexpected weight loss
- Bloody stools
- Vomiting
It is also important to note that unless the condition becomes severe, the symptoms of Barrett's oesophagus are similar to those of acid reflux.
Is it GERD or something else?
Sometimes, the symptoms of GERD may overlap with other conditions or be described with confusing terminology. Some examples include heartburn and acid reflux. Some patients may even suffer from functional dyspepsia (functional digestive disorder) that may overlap with GERD.
Therefore, if you are seeking to get diagnosed properly, it is wise to consult an experienced gastroenterologist to thoroughly assess you and determine if you have GERD, acid reflux, or heartburn in Singapore.
How is GERD diagnosed?
Apart from a physical examination, your gastroenterologist may recommend several other investigations to confirm the diagnosis, including the following:
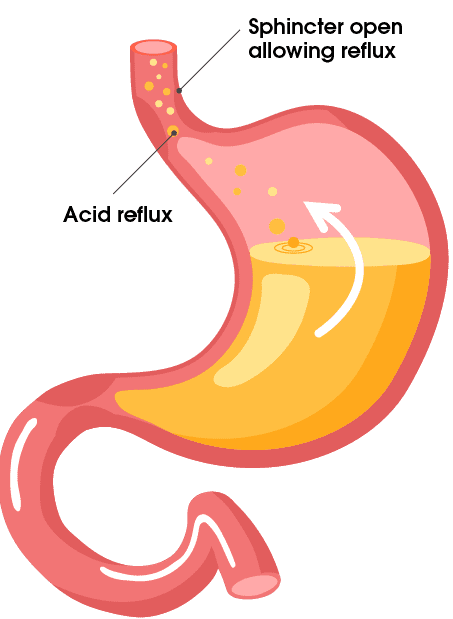
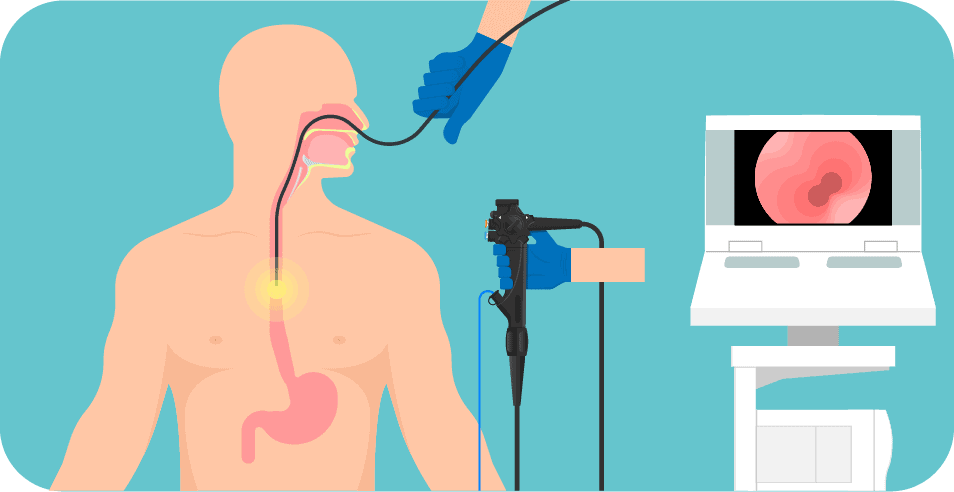
Gastroscopy
A gastroscopy, also known as an Oesophago-Gastro-Duodenoscopy (OGD), allows the gastroenterologist to examine the upper gastrointestinal (GI) tract for any structural abnormalities. It involves the insertion of an endoscope into your throat and the duodenum.
An endoscopy can also be used for a biopsy, where a small part of the oesophagus is collected and tested for other conditions, such as Barrett’s oesophagus or oesophageal cancer.
Ambulatory (24 hours) Oesophageal pH Test
A catheter containing a pH probe is inserted through the nose and positioned five cm above the LOS for 24 hours to record changes in acid reflux with regard to your meals and other daily activities.
If the catheter feels extremely uncomfortable, your gastroenterologist may recommend a wireless capsule which is endoscopically inserted and positioned at the same location. Since the capsule can transmit data while attached, no retrieval process is needed, and it can be passed out and then disposed of immediately after the test.
Oesophageal Manometry
After numbing medication is applied (in and around the nose and throat), a catheter is inserted into the oesophagus through your nose. Your gastroenterologist will then ask you to swallow small sips of water, and a computer connected to the catheter will measure the speed, pattern and strength of your oesophageal muscle contractions.
X-ray
Barium contrast radiography is an X-ray study that involves the ingestion of barium pills (or solution) that coats the oesophagus and alimentary tract, making it easier for your gastroenterologist to see the silhouette of the tract and detect any abnormalities.
Can GERD be cured?

If pregnancy and obesity are the underlying causes of your GERD, the symptoms will resolve when medication is taken along with weight management for obesity. In the case of a pregnancy, medicines such as antacids may be prescribed to relieve symptoms. However, in most cases, the associated symptoms will dissipate once the woman gives birth.
Generally, surgery is only recommended when patients with GERD do not respond to medication or if complications such as cancer have occurred. Otherwise, medication can be prescribed along with proper lifestyle management.
What are the treatments for GERD in Singapore?
Lifestyle Changes
For those with mild GERD, lifestyle changes may easily help reverse the damage caused. These changes include:
- Quitting smoking
- Losing weight
- Eating smaller meals
- Sitting upright for a few hours after every meal
- Avoiding alcohol intake
- Reducing pressure on the stomach
Foods to avoid:
- Fatty and oily food and beverage
- Spicy food
- Citruses
- Carbonated drinks
- Tomato and tomato-based foods
- Fried food
- Onion and garlic
- Mint
- Chocolate
- Coffee

These foods are thought to worsen GERD by increasing the acidity of your stomach. They may also irritate the oesophagus lining. Hence, it would be best to reduce the consumption of these foods if you have GERD.
Medication

When lifestyle and diet changes are not enough to cure GERD, your gastroenterologist may prescribe medicines like proton pump inhibitors (PPI), antacids or H2-receptor antagonists (H2RAs) to treat GERD.
Proton Pump Inhibitors (PPI)
PPIs block and reduce the production of stomach acid to reduce the severity and frequency of acid reflux. This gives the oesophageal tissue time to heal, aiding with the reduction and prevention of heartburn.
Antacids
Antacids neutralise stomach acid, making the stomach contents less corrosive. This provides short-term relief for acid reflux.
Histamine 2 Receptor Antagonists (H2RAs)
H2RAs decrease the production of stomach acid by reversibly binding to histamine receptors and blocking the production of histamine on gastric parietal cells in the stomach. This is helpful because histamines play a role in stimulating the secretion of stomach acid (gastric acid). This reduction of gastric acid production will help reduce the effects of acid reflux.
Surgery
Surgery may be required if medication and lifestyle changes fail to alleviate your GERD symptoms.
Surgical therapy for GERD in Singapore can be laparoscopic or endoscopic, both of which are less invasive compared to traditional open surgery.
- Laparoscopic surgery – This procedure allows small incisions to be made for surgical tools to be inserted into the body to carry out the surgery.
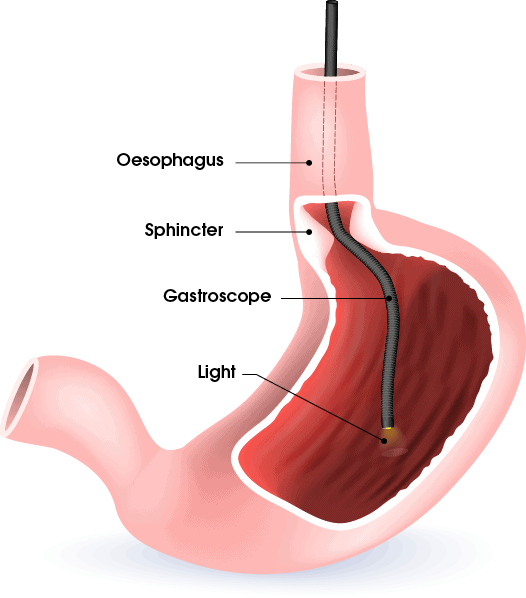
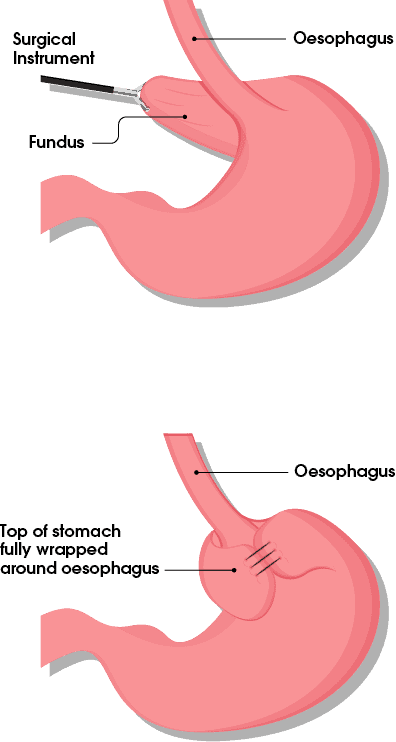
- Nissen fundoplication:
- Part of the upper stomach is wrapped around the LOS, tightening the sphincter and preventing acid reflux.
- Anterior partial fundoplication:
- It is similar to Nissen fundoplication, except that the upper portion of the stomach only wraps around part of the oesophagus.
- Magnetic sphincter augmentation (MSA)
- A small device made of tiny magnetic titanium beads (LINX) is implanted into the sphincter, strengthening it.
- Bariatric surgery
- For obese patients
- Helps reduce the size of meals they eat and the pressure on their stomachs.
- Nissen fundoplication:
- Endoscopic surgery (endoluminal therapy) – Surgical tools are attached to the endoscope, which is inserted into the oesophagus through the mouth.
- Transoral incisionless fundoplication (TIF):
- A TIF device is attached to the endoscope, which allows the doctor to repair or re-create the LOS such that it becomes a stronger barrier against acid reflux.
- A TIF device is attached to the endoscope, which allows the doctor to repair or re-create the LOS such that it becomes a stronger barrier against acid reflux.
- Endoscopic radiofrequency (RF) ablation
- This non-invasive procedure involves the use of a balloon catheter with four needle electrodes being deployed when inflated. The low-energy radiofrequency pulses emitted by the electrodes help strengthen the sphincter without causing any damage to the surrounding tissue.
- Transoral incisionless fundoplication (TIF):
What complications can arise if GERD is left untreated?
As mentioned before, while GERD is not directly linked to the development of oesophageal cancer, patients with Barrett’s oesophagus are at a higher risk of progressing to oesophageal adenocarcinoma.
Untreated GERD can lead to other complications, such as oesophagitis, which is the inflammation of the oesophagus lining. This may result in bleeding, ulcers and painful swallowing.
Hence, if you suspect that you have GERD and are unable to resolve its symptoms with over-the-counter medications and lifestyle changes, do seek medical attention from a gastroenterologist in Singapore.
When should I contact a Gastroenterologist?
If you experience GERD symptoms such as chronic acid reflux, please consult your gastroenterologist, as they may be a sign that GERD complications have set in. More importantly, keep a lookout for the following symptoms:
- Recurrent vomiting episodes
- Difficulty swallowing
- Sudden unexplained weight loss
- Black or tarry stools (indicates bleeding)
If you notice that you have bloody stools, you may take a photo to show your gastroenterologist.
Summary
“GERD is a very common gastrointestinal condition that can often be treated with a combination of lifestyle modifications and medications. However, if your symptoms persist or if you have any of the red flag symptoms highlighted in the article, it is advisable to consult a gastroenterologist for further evaluation”, advises Dr Benjamin Yip.
A gastroscopy could be conducted to check for any structural abnormalities, such as the presence of erosions, ulcers or changes in the oesophagus. That being said, prevention is always better than cure. Small things you can do to prevent GERD include refraining from eating two hours before bedtime, quitting smoking, losing weight and refraining from alcohol. Following these good habits and practices will decrease your risk of developing GERD. For more information on how to manage your GERD, heartburn, or acid reflux in Singapore, do get in touch with our team at Alpha Digestive & Liver Centre. We would be more than happy to help you.
References
- Bhargava, H. D. (2020, September 11). GERD: Symptoms, Causes, Treatments, Remedies for Relief. WebMD. Retrieved April 22, 2022, from https://www.webmd.com/heartburn-gerd/guide/reflux-disease-gerd-1
- Fass, R. (n.d.). Causes of GERD. About GERD. Retrieved April 22, 2022, from https://aboutgerd.org/what-is/introduction-to-gerd/causes-of-gerd/
- Gastroesophageal reflux disease (GERD) - Symptoms and causes. (2020, May 22). Mayo Clinic. Retrieved April 22, 2022, from https://www.mayoclinic.org/diseases-conditions/gerd/symptoms-causes/syc-20361940
- Gastroesophageal Reflux Disease Symptoms, Diagnosis & Treatment. (n.d.). American Academy of Allergy, Asthma & Immunology. Retrieved April 22, 2022, from https://www.aaaai.org/Conditions-Treatments/related-conditions/gastroesophageal-reflux-disease
- GERD: Can certain medications make it worse? (n.d.). Mayo Clinic. Retrieved April 22, 2022, from https://www.mayoclinic.org/diseases-conditions/gerd/expert-answers/heartburn-gerd/faq-20058535
- GERD (Chronic Acid Reflux): Symptoms, Treatment, & Causes. (2019, December 6). Cleveland Clinic. Retrieved April 22, 2022, from https://my.clevelandclinic.org/health/diseases/17019-gerd-or-acid-reflux-or-heartburn-overview
- Gotfried, J., & Katz, L. (n.d.). Ambulatory pH Monitoring - Gastrointestinal Disorders - MSD Manual Professional Edition. MSD Manuals. Retrieved April 26, 2022, from https://www.msdmanuals.com/en-sg/professional/gastrointestinal-disorders/diagnostic-and-therapeutic-gastrointestinal-procedures/ambulatory-ph-monitoring
- H2 Receptor Antagonist (H2RA) and Proton Pump Inhibitors (PPI) - Chambers' Apothecary. (2016, August 29). Chambers Apothecary. Retrieved April 26, 2022, from https://www.chambersapothecary.com/blog/2016/08/29/h2-receptor-antagonist-h2ra-and-proton-pump-inhibitors-ppi/
- Gastroesophageal Reflux Disease in Asia: A historical perspective and present challenges. Wiley Online Library (2011, January 04). Retrieved October 31, 2023, from https://onlinelibrary.wiley.com/doi/full/10.1111/j.1440-1746.2010.06534.x#:~:text=In%20a%20survey%20of%20more,of%20reflux%20esophagitis%20of%203.3%25
- J.Arts, J. Tack, J.P. Galmiche. Endoscopic Antireflux Procedures. National Library of Medicine (2004, August). Retrieved October 31, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1774149/
- Alyssa Anderson. What is Stretta? WebMD. Retrieved October 31, 2023 from https://www.webmd.com/heartburn-gerd/what-is-stretta

