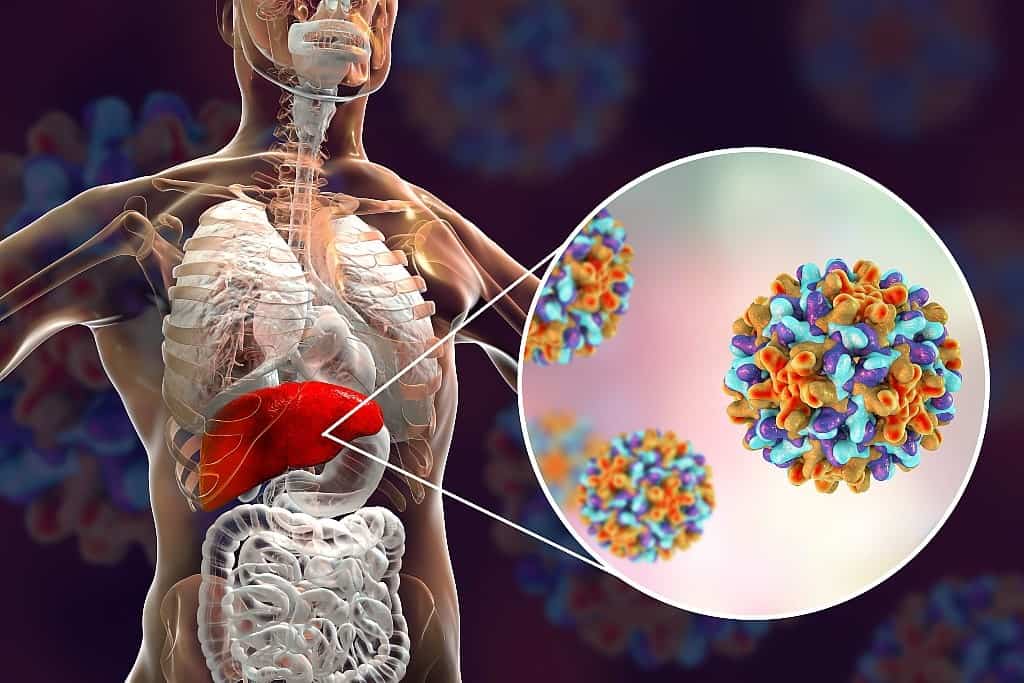
What is Viral Hepatitis?
Hepatitis is the inflammation of the liver. Viral hepatitis is a commonly known infection in Singapore which causes inflammation and swelling of the liver, affecting liver function and its ability to regenerate. This could be due to various strains of viruses such as hepatitis A, B, C, D and E.
What are the types of Viral Hepatitis?
Hepatitis A
Hepatitis A is usually self-limiting in that most patients recover on their own. Most recover from the infection within days or weeks without medical intervention.
What causes Hepatitis A?
Ingesting food and beverages contaminated with the hepatitis A virus or consuming raw vegetables, shellfish, and other foods will increase your risk of contracting Hepatitis A.
Hepatitis B
Hepatitis B is the number one cause of liver cancer. Roughly one million people die every year from Hepatitis B, even though it is highly preventable.
What causes Hepatitis B?
This virus is transmitted through contact with infected blood or bodily fluids. Hepatitis B can also be transmitted from a pregnant mother to her unborn child in her womb.
Hepatitis C
About 80% of Hepatitis C carriers develop chronic viral hepatitis. While curable in its early stages, this condition typically goes unnoticed until the virus has badly damaged the liver. By then, it is usually much harder to treat Hepatitis C.
What causes Hepatitis C?
The hepatitis C virus is transmitted through contact with infected blood, contaminated needles and from a pregnant mother to her unborn child in her womb.
Hepatitis D
This condition is relatively rare compared to the other types of viral hepatitis. This is because the hepatitis D virus can only infect people who have the hepatitis B virus in their bodies.
What causes Hepatitis D?
Hepatitis D is transmitted via blood transfers between infected and non-infected people, sharing of needles and syringes, and from infected mothers to unborn babies in their wombs.
This transmission can only occur if the recipient already has chronic Hepatitis B (superinfection) or is simultaneously infected with the hepatitis B virus (coinfection).
Hepatitis E
Hepatitis E is also a self-limiting form of viral hepatitis and is commonly found in East and South Asia. Medical intervention is usually not needed for those with Hepatitis E as it will resolve on its own in about 4-6 weeks.
However, for immunosuppressed individuals or pregnant women, there is an increased risk of Hepatitis E leading to more severe complications.
What causes Hepatitis E?
Similar to Hepatitis A, Hepatitis E is transmitted through the consumption of raw vegetables, shellfish and other foods. Hence, good sanitation, good hygiene practices, and adequately cooking your food will help prevent Hepatitis E.
How does Viral Hepatitis affect my liver?

Viral hepatitis attacks liver cells, causing acute or chronic inflammation. This eventually leads to the formation of scar tissue (fibrosis), causing the liver to stiffen.
Chronic inflammation leads to liver damage, affecting the liver’s ability to function and regenerate. This can result in life-threatening conditions such as liver failure or liver cancer.
Can Viral Hepatitis be cured?
Viral hepatitis can be acute or chronic.
Acute viral hepatitis can go away on its own and requires no treatment. For chronic viral hepatitis B, there is generally no cure. However, treatment can help manage and control the condition to prevent further complications such as cirrhosis, liver failure, and liver cancer. For chronic hepatitis C, there are several new medications that can offer very good cure rates.
What are the symptoms of Viral Hepatitis?

Common symptoms of viral hepatitis include:
- Fever
- Joint pain or joint stiffness
- Rash
- Swelling of the legs
- Fatigue
- Muscle pain
- Anorexia
- Nausea and/or vomiting
- Abdominal pain
- Diarrhoea
- Dark urine
- Clay-coloured stool :
- Yellowing of the skin and whites of the eyes (jaundice)
- Skin lesions
When will these symptoms develop?
The time for symptoms to develop varies with the type of virus causing the disease.
- Hepatitis A: 2-7 weeks after infection
- Hepatitis B: 6 weeks to 6 months after infection
- Hepatitis C: 6-7 weeks after infection
- Hepatitis D: 3-7 weeks after infection
- Hepatitis E: 2-9 weeks after infection
Developing symptoms are usually a telltale sign that your viral hepatitis has progressed to something more severe.
Hence, if you have been tested positive for viral hepatitis or have come into contact with an infected individual, do keep a lookout for symptoms during the next six months and consult a doctor immediately if they surface.
How is Viral Hepatitis diagnosed?
Your gastroenterologist diagnoses viral hepatitis by analysing your symptoms, and conducting a physical exam and blood tests. Sometimes, they may order imaging tests and a liver biopsy to assess if the infection has progressed to more serious conditions like liver cirrhosis (scarring of the liver) or liver cancer.
Blood tests
A blood test includes a serology test. The serology test looks for antibodies produced by your body in your bloodstream.
Through the blood test, your gastroenterologist may be able to tell the severity of the infection, the viral strand you have, if you are contagious and whether the viral infection is acute or chronic.
Ultrasound
An ultrasound is a diagnostic tool which utilises high-frequency sound waves to create a 2-dimensional (2D) image of your liver. This scan will help your gastroenterologist detect structural abnormalities in the liver and assess the extent of damage caused by the infection.
Transient Elastography
Transient elastography is a non-invasive and inexpensive diagnostic test for liver fibrosis. Using a FibroScan probe, low-frequency vibrations are emitted at your liver area to generate a liver stiffness score. This score will tell your gastroenterologist the extent of liver fibrosis in your liver.
Magnetic Resonance Elastography (MRE)
An MRE uses low-frequency vibrations to generate cross-sectional images of the liver. This allows your gastroenterologist to assess for any structural abnormalities and stiffness of liver tissue.
Liver Biopsy
Liver biopsies are recommended to assess the extent of fibrosis and rule out other causes of hepatitis. This involves the extraction of a small portion of your liver using a fine, hollow needle.
The tissue sample retrieved will be sent to a pathologist who helps determine the extent and distribution of inflammation and fibrosis. This information will help your gastroenterologist accurately determine your treatment plan.
How is Viral Hepatitis treated?
Treatment for viral hepatitis depends on the type of viral strand you have and the severity of your infection.
Early stages
Generally, in the early stages of viral hepatitis, antiviral medication is prescribed to help slow the progression of infection and reduce damage caused to the liver.
Examples of these antiviral medications are:
- Entecavir
- Tenofovir
- Sofosbuvir/velpatasvir (Epclusa)
- Gleclaprevir/pibrentasvir (Mavyret)
- Ribavirin
Advanced stages
When viral hepatitis progresses to advanced liver cirrhosis, previously listed medications can still be given to prevent further damage to the liver. This typically occurs in patients with chronic Hepatitis B, C and D.
Medication
New medications will be given to treat complications which may arise once the patient develops liver cirrhosis:
- Diuretics — when your liver is dysfunctional, excess fluid builds up in the abdominal area (ascites). Diuretics and a low salt diet will help drain the liquid and relieve pressure.
- Propranolol or carvedilol — severe liver scarring causes high blood pressure in the portal vein, and blood is directed away from the liver. Propranolol and isosorbide help reduce this high blood pressure.
- Antibiotics and laxatives — liver failure can lead to a build-up of toxins in the liver. These metabolic toxins are flushed out using antibiotics and laxatives.
Procedures
Portal hypertension refers to high pressure in the vein leading to the liver. It is a common complication of viral hepatitis where the pressure can cause backflow of blood into smaller vessels found elsewhere, resulting in varices or enlarged veins at those locations.
Varices are dangerous as they can start bleeding and cause hypovolemic shock. Treatment can involve procedures such as:
- Band Ligation – Endoscopy is used to find the site of bleeding. Once the bleeding vein is found, a rubber band is used to close it.
- Transjugular Intrahepatic Portosystemic Shunting – The portal and hepatic veins of the liver are surgically connected using a stent. This relieves blood pressure in the liver and allows blood to flow normally around your body again.
- Paracentesis – Removal of excess fluid in the abdomen via a needle.
In the worst-case scenario, where you have unsalvageable liver failure or end-stage liver disease, a liver transplant might be needed. Your new liver may come from two different sources:
- Your liver may be replaced by half a liver from a living donor. The liver then grows to normal size in both you and the donor after surgery
- Your liver may be replaced by a normal-sized liver from a deceased person
What happens if Viral Hepatitis is left untreated?
Viral hepatitis can be split into two kinds: acute and chronic.
If you leave acute viral hepatitis untreated, you generally do not suffer any complications as it can resolve on its own. However, in rare cases, acute hepatitis can quickly progress to liver failure (fulminant viral hepatitis).
If you leave chronic viral hepatitis untreated, the infection usually progresses to liver scarring (liver cirrhosis) and then liver failure. When too much of the liver is scarred, the liver is no longer able to regenerate and becomes dysfunctional.
Since one is usually unable to tell which kind of viral hepatitis one has, it is best to seek medical treatment the moment you suspect you have the virus. Doing so will prevent the infection from progressing and protect you from complications of the virus (if any).
What is Fulminant Hepatitis?
Fulminant Hepatitis is a form of acute viral hepatitis where the death of liver tissue and reduction in liver size occurs in an abnormally short period of time. This rare condition occurs in up to 1% of viral Hepatitis A or B cases where about half are caused by a hepatitis D virus coinfection. Occasionally, the hepatitis E virus also leads to Fulminant Hepatitis.
As a result of how quickly the liver deteriorates and becomes dysfunctional, emergency medical treatment is needed immediately upon detection of symptoms. Antiviral medication is usually used to treat it, followed by liver transplants if the condition escalates too quickly.
Symptoms of this condition are similar to those of regular viral hepatitis.
Can Viral Hepatitis be prevented?

Viral hepatitis A and B can be prevented via vaccinations.
Hepatitis A
In Singapore, vaccinations against Hepatitis A are not given at birth. Instead, Singaporeans are expected to book a vaccination appointment for themselves when going to a country where Hepatitis A is rampant.
Immunity lasts for 14-20 years in children and at least 25 years in adults.
Hepatitis B
In Singapore, vaccines for Hepatitis B are usually given at birth
Immunity usually lasts for up to 15 years after vaccination, after which a second round of vaccination will have to be taken again.
For Hepatitis C and D, vaccines are unavailable. For hepatitis E, vaccines are being developed.
Living with Viral Hepatitis
Apart from taking medication, lifestyle changes are also an effective way to manage viral hepatitis. These include:
- Do not consume alcohol
- Avoid overuse of certain medications like acetaminophen or Panadol
- Reduce smoking
- Check with your gastroenterologist before taking any health supplements
Apart from taking steps to protect your health, you can also adopt new hygiene practices to avoid spreading viral Hepatitis to others. Such practices include:
- Washing your hands with soap and water after using the bathroom or changing diapers, and before eating
- Do not prepare or cook food unless your gastroenterologist deems it safe to do so
- Have a set of household utensils for your private use
- Avoid injected drug use and sharing of needles
- Tell close contacts about your condition so they can take necessary precautions
- Never donate blood, organs or tissue
- Abstain from sex or use condoms
- Limit the number of sexual partners you have
- Do not share personal items that may have bodily fluid on them:
- Razors, toothbrushes, pierced earrings
Summary
Most viral hepatitis can be managed to prevent further complications. Since the virus can also cause asymptomatic infections, you should go for checkups when you come into contact with a carrier, when you are pregnant, or if you have visited a place where viral hepatitis is very common. To further lower your risk of suffering complications from the virus, take all required vaccinations and maintain proper hygiene wherever you go.
A gentle reminder from Dr Benjamin Yip: Viral hepatitis is a relatively common problem with various causes. The tests needed to diagnose these conditions are also fairly numerous and complex. If in doubt, always consult your Gastroenterologist!

