What is Gastrointestinal Cancer?
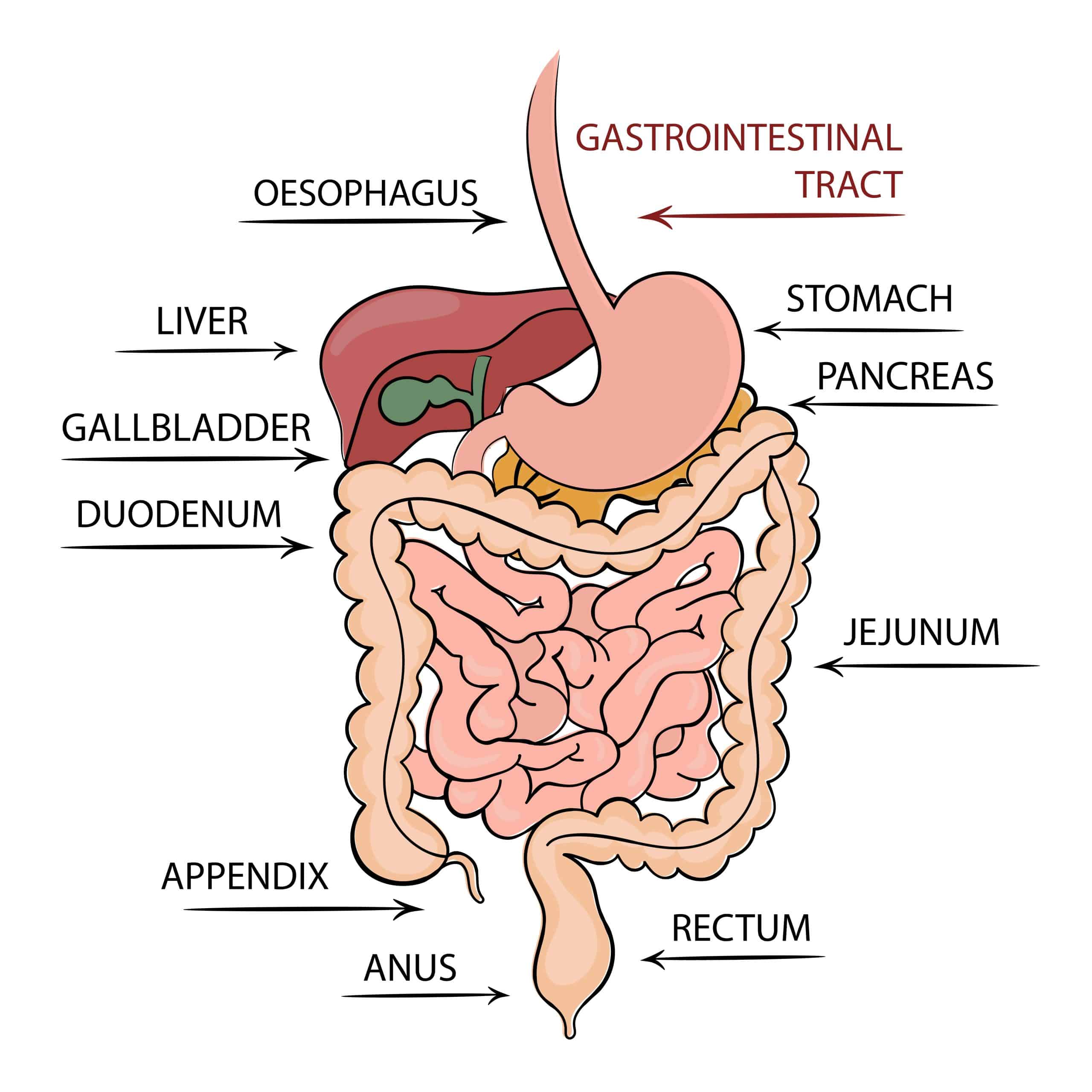
The gastrointestinal (GI) tract is about 25 to 30 feet long and extends from the mouth to the anus. It consists of the oral cavity, pharynx, oesophagus, stomach, small intestine, large intestine (colon), and rectum, which helps with digesting the ingested nutrients and excreting the waste products of digestion. The GI tract also comprises glandular organs that aid digestion, such as the salivary glands, pancreas, liver and biliary system.
GI cancer arises when various DNA mutations or defects cause abnormal and unregulated cell growth in various locations of the GI tract, forming a tumour. Gastrointestinal cancer has a multitude of possible causes, including certain underlying medical conditions and various other risk factors such as a family history of gastrointestinal cancer, unhealthy diet and lifestyle choices.
Which Gastrointestinal Cancer is the most common?
Based on the Singapore Cancer Registry’s latest Annual Report (2017-2021), colorectal cancer is the most common type of gastrointestinal cancer in Singapore, comprising 16.3% of cancers in men and 12.9% of cancers in women. Liver and stomach cancer are the 2nd and 3rd most common gastrointestinal cancers, with a prevalence of 7.3% in men and 6.2% in women for liver cancer and a prevalence of 4.1% in men and 4.7% in women for stomach cancer.
Which Gastrointestinal Cancer is the most fatal?
Colorectal cancer, being the most common gastrointestinal cancer, also has the highest absolute number of deaths, accounting for 14.4% of all cancer-related deaths in men and 15.6% in women.
However, among the most common cancers for 2015-2019, pancreatic and liver cancer had the poorest 5-year survival rates for males (12.2% and 25.5%, respectively), while stomach cancer had the lowest survival rates for females at 39.7%.
Pancreatic cancer: The silent killer
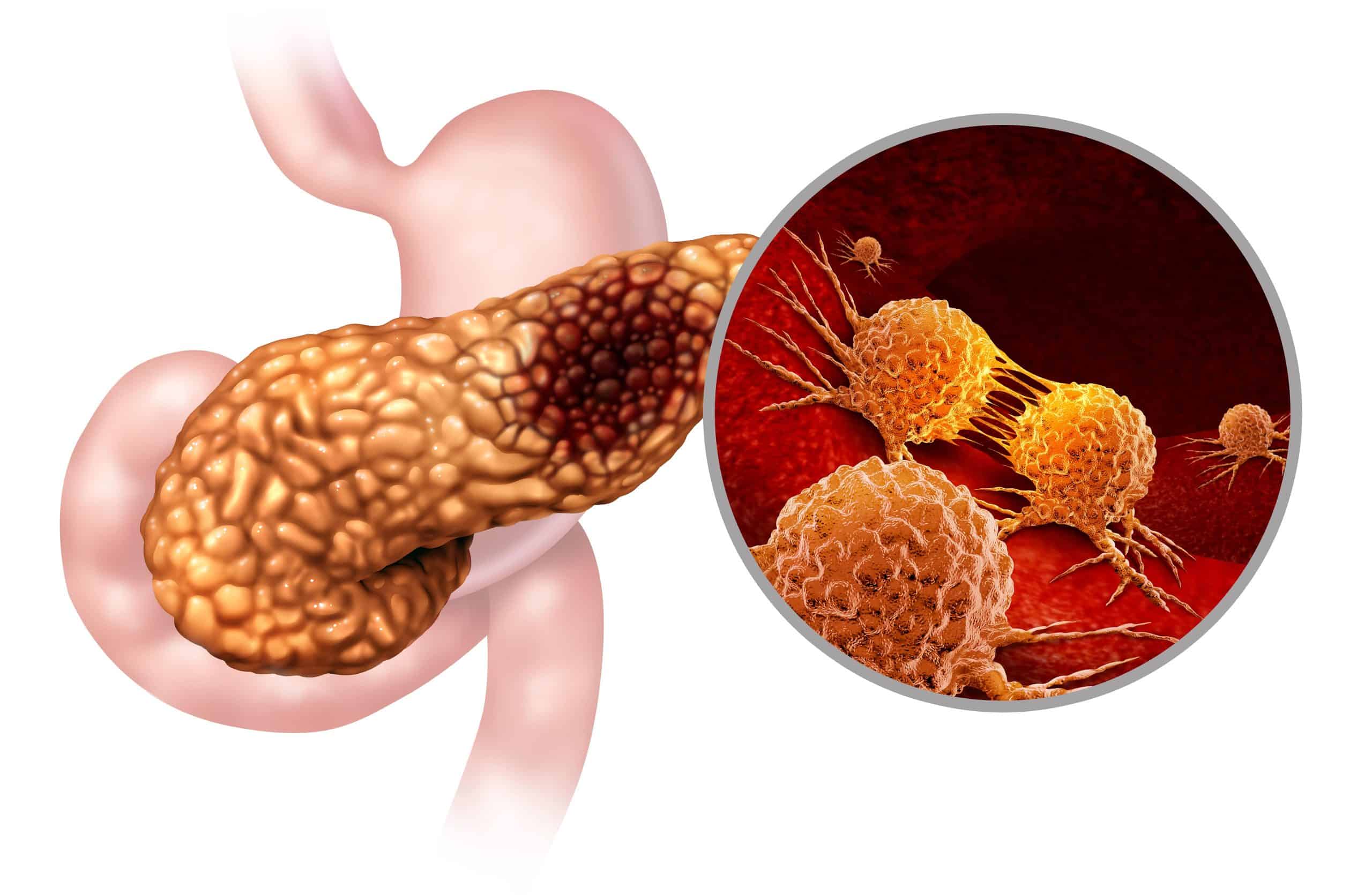
While both stomach and pancreatic cancer account for the poorest 5-year survival rate in patients, pancreatic cancer is usually considered to be more deadly as there are no definitive screening tests to catch it in its early stages compared to stomach cancer.
Although relatively rare, pancreatic cancer is a silent killer as it is hard to detect until it has reached late stages or spread, resulting in some of the highest mortality rates of all cancers. Additionally, pancreatic cancer does not respond as well to commonly used cancer treatment, so there are fewer treatment options. This treatment resistance is largely due to the development of an immune-suppressed microenvironment that prevents the local immune system from clearing the tumour.
In Singapore, it accounted for 3.2% of cancers in men and <2.8% in women, with 6.3% of cancer deaths in men and 6.7% in women in 2019. This means that despite the relatively lower prevalence of this cancer, it has a disproportionately high mortality rate.
On a positive note, early-stage gastrointestinal cancers tend to have better recovery outcomes, which underscores the importance of seeking an early diagnosis and starting treatment promptly.
How quickly does each cancer spread?
The rate of spread depends on the type of cancer and its aggressiveness, and varies greatly depending on the underlying mutations. It can range from months in extremely aggressive cancers, to years in slow-growing cancers.
The ‘slow-growing’ types take years to develop into a sizeable tumour that may cause symptoms. Hence it is important for patients to undergo regular endoscopic screening for cancers such as stomach and colorectal cancer enabling any pre-cancerous masses to be detected early.
What are the Symptoms of Gastrointestinal Cancer?

General symptoms of gastrointestinal cancer include fatigue, unintentional loss of weight and loss of appetite. Each type of gastrointestinal cancer has its own unique symptoms, which we will briefly cover below:
Oesophageal Cancer
- Dysphagia (difficulty swallowing) - solid food, then liquids later on
- Cough
- Vomiting after meals
- Hoarse voice
Stomach/Gastric Cancer
- Abdominal bloating, pain or discomfort
- Nausea/vomiting
- Loss of appetite
- Bleeding (vomiting blood or passing out blood in stools)
- Early satiety (the sensation of being full after eating very little)
Colorectal Cancer
- Abdominal pain
- Blood coating the stools or mixed inside
- Altered bowel habits (constipation, diarrhoea, or both)
- A change in stool calibre or shape
- Sensation of incomplete defecation
Liver Cancer (Hepatocellular Carcinoma)
- Abdominal pain
- Jaundice (yellowed appearance of skin or eyes)
- Ascites (fluid accumulation in the abdomen)
Pancreatic Cancer
- Abdominal or lower back pain
- Jaundice (yellowed appearance of skin or eyes)
What are the Causes of Gastrointestinal Cancer?
There is no single cause for any type of cancer, and gastrointestinal cancer is no exception. Listed below are the most common causes for each type of gastrointestinal cancer.
Oesophageal Cancer
While there is no definitive cause for oesophageal cancer, the following may contribute to its development.
- Obesity
- Smoking
- Alcohol consumption
- A family history of oesophageal cancer
- Underlying medical conditions (e.g., Barrett’s oesophagus)
- Exposure to certain chemical fumes
Stomach Cancer
Here are some factors that may put you at risk of developing stomach cancer:
- Obesity
- A diet rich in salt and smoked foods
- Smoking
- Alcohol consumption
- Polyps
- Stomach infection (e.g., helicobacter pylori)
- A family history of stomach cancer
- A family history of genetic syndromes (e.g., familial adenomatous polyposis, juvenile polyposis syndrome, etc.)
- Underlying gastric conditions (e.g., gastroesophageal reflux disease)
Liver Cancer
The most common factors that can increase the risk of liver cancer, including the following:
- Chronic hepatitis (Hepatitis B or C)
- Obesity
- Smoking
- Alcohol consumption
- Underlying medical conditions (e.g., Diabetes, cirrhosis, nonalcoholic fatty liver disease, etc.)
Pancreatic Cancer
The following factors can make you more susceptible to developing pancreatic cancer:
- Age (over 60)
- Diabetes
- Chronic pancreatitis
- Obesity
- Smoking
- Alcohol consumption
- A family history of pancreatic cancer
What are the tests used to diagnose Gastrointestinal Cancer?
Oesophageal, gastric and colorectal cancers may be diagnosed through endoscopic procedures, such as Oesophago-Gastro-Duodenoscopy (OGD), to visualise the upper GI tract (oesophagus, stomach, part of the small intestine), and colonoscopy for the lower GI tract (large intestine, rectum). Even in the absence of symptoms, endoscopic screening is recommended for adults starting from the age of 50 (or earlier if one has risk factors, which your doctor will advise you on).
An endoscopy is done by inserting a flexible, thin tube with a camera attached to the end down your throat (in an OGD) or through the anus in a colonoscopy. This enables your doctor to visualise the appearance of your gastrointestinal tract and take samples of your tissue if required. Any inflammation, bleeding or abnormal masses can be easily seen, and biopsies (tissue samples) will be taken for further testing (if needed) to confirm the diagnosis of cancer.
Diagnosis for liver or pancreatic cancer
For liver or pancreatic cancer, since both organs are unable to be visualised via endoscopy, a computerised tomography (CT) scans or Magnetic Resonance Imaging (MRI) are usually done. A CT scan combines multiple X-ray images into a computer system which generates cross-sectional images of your body, whereas an MRI uses strong magnets and radio waves.
Cancer is diagnosed based on histology (appearance of cells under the microscope), while staging is determined by the TNM system (Tumour-Nodes-Metastasis).
To determine the stage, a CT Thorax-Abdomen-Pelvis is commonly done to assess the size of the tumour, depth of invasion, and whether it has spread to adjacent organs or lymph nodes.
If there is suspicion of lymph node invasion, a fine needle aspiration cytology (FNAC) or biopsy (FNAB) may be performed on the lymph node. It involves inserting a needle into the lymph node (under local anaesthesia) to withdraw tissue samples for further examination under the microscope, to determine the presence of cancer cells.
This is just a general overview of commonly used diagnostic tests; your doctor will tailor the tests and scans according to the type and location of cancer.
Is it Cancer or Irritable Bowel Syndrome (IBS)?
The symptoms of colorectal cancer and IBS have some overlap, with both having:
- Abdominal cramps, pain or discomfort
- Altered appearance of stools (eg. constipation, diarrhoea, mixed, mucoid)
- Bloating
- Sensation of incomplete defaecation
However, colorectal cancer has additional concerning symptoms like blood in stools, a change in stool calibre or shape, unexplained weight loss or loss of appetite.
How do I know if I have Gastritis or Cancer?
Gastric cancer and gastritis have some similar symptoms, and they are as follows:
- Early satiety (feeling full soon after eating)
- Abdominal pain and cramps
- Indigestion
- Nausea/vomiting
Gastric cancer is more prevalent in Asia than in Western countries, accounting for 50% of stomach cancer cases worldwide. It is thought to be associated with Helicobacter Pylori infection, a bacterial infection that causes gastritis/duodenitis and stomach/duodenum ulcers. Additionally, chronic gastritis may damage the stomach lining, marginally increasing your risk of gastric cancer.
Is Gastrointestinal Cancer curable?
Depending on the stage at which the cancer is diagnosed, it may or may not be curable. For instance, in an early stage when the tumour is relatively small and has not spread beyond the organ itself, it may be curable after surgical removal of the tumour and chemotherapy/radiotherapy.
However, in late-stage cancers, when the tumour is too large to be removed safely or has spread to other parts of the body (metastatic cancer), there is a poorer prognosis. Treatment for those with late-stage stomach cancer will be focused on managing symptoms, reducing pain and discomfort, or shrinking the tumour, but it cannot be cured.
What are the Treatments available for Gastrointestinal Cancer?

The aim of cancer treatment can be to cure and achieve control or to palliate symptoms and provide comfort care. Gastrointestinal cancer treatment will vary from patient to patient and is personalised according to the type and stage of cancer, the patient’s choice, and long-term care goals, and should be discussed in detail with your Gastroenterologist and family members.
If the goal is to cure the cancer, surgery is done to remove or reduce the size of the tumour and used in combination with either chemotherapy or radiotherapy, which kill or reduce the further proliferation of cancer cells. Once the surgeon has determined that there are minimal remaining cancer cells, the patient will continue with regular doctor’s appointments to undergo blood tests and surveillance scans to check for any recurrence.
If the cancer is determined to be too advanced to be cured, palliative treatment is typically provided to ease distressing symptoms and enhance quality of life. Surgery, chemotherapy or radiotherapy may be offered to relieve the symptoms of a large tumour, but the goal is not to cure or remove it entirely. Pain management is a key aspect of palliative care, with options such as analgesics and nerve blocks being used to alleviate pain.
How can I reduce my risk of developing Gastrointestinal Cancer?
There are various risk factors for developing cancer, such as a family history of similar cancers, chronic inflammatory diseases, an unhealthy diet, smoking, excessive alcohol consumption, etc. While some risk factors are non-modifiable, one can reduce the risk of cancer by cutting down on alcohol intake and smoking, having a healthy diet, and attending routine health screenings to ensure that any cancers are detected in the earlier stages.
When it comes to gastrointestinal cancers, there is an array of screening modalities to help with detection, such as gastroscopy, colonoscopy, stool samples, faecal immunochemical test (FIT), GASTROClear, and other tests. Although colorectal cancer screening tests are commonly carried out in Singapore, gastric cancer screening isn’t typically performed. However, Dr Benjamin Yip advises patients to undergo gastric screening as well as it can strike at a young age (early 30s and older), making early detection an important component in achieving a good prognosis.
Living with Gastrointestinal Cancer

While the diagnosis of cancer is certainly concerning and stressful, it is not always a death sentence. With a rigorous treatment regime, regular scans and frequent appointments with your doctor, it is possible to manage the disease and its symptoms, and potentially go into remission. Psychological support for the patient and their family is also essential in getting through such health challenges.
Summary
In conclusion, there are many types of gastrointestinal cancers, each with its unique symptoms and risk factors. On top of leading a healthy lifestyle, it is essential to undergo regular health screenings and highlight new, unexplained symptoms to your Gastroenterologist so that any diseases can be discovered and treated as early as possible.
Visit Alpha Digestive & Liver Centre
If you have symptoms of gastrointestinal cancer, such as fatigue, unintentional loss of weight and loss of appetite, it is advisable to book an appointment with our Gastroenterologist Dr Benjamin Yip for an early diagnosis.
References
- https://journals.lww.com/ajg/pages/articleviewer.aspx?year=2021&issue=03000&article=00014&type=Fulltext. Accessed 25 July 2022.
- “Cancer Statistics.” National Cancer Centre Singapore, 8 March 2022, https://www.nccs.com.sg/patient-care/cancer-types/cancer-statistics. Accessed 25 July 2022.
- “Gastrointestinal Cancers.” American College of Gastroenterology, https://gi.org/topics/gastrointestinal-cancers/. Accessed 25 July 2022.
- “Singapore Cancer Registry Annual Report 2019.” National Registry Of Diseases Office, 28 January 2022, https://www.nrdo.gov.sg/docs/librariesprovider3/default-document-library/scr-2019_annual-report_final.pdf?sfvrsn=fa847590_0. Accessed 25 July 2022.
- “Stomach cancer incidence rates among Americans, Asian Americans and Native Asians from 1988 to 2011.” NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4430761/. Accessed 25 July 2022.
- “Singapore Cancer Registry Annual Report 2021”, Health Promotion Board. https://www.nrdo.gov.sg/docs/librariesprovider3/default-document-library/scr-ar-2021-web-report.pdf?sfvrsn=591fc02c_0 Accessed 22 December 2023
- “Gastrointestinal Cancer”, ScienceDirect. https://www.sciencedirect.com/topics/neuroscience/gastrointestinal-cancer Accessed 22 December 2023

