What are Pancreatic Cysts?
Pancreatic cysts are fluid-filled sacs on or in the pancreas. The pancreas is a large organ behind the stomach responsible for producing hormones and enzymes that assist in the digestion of food. The pancreas plays a vital role in digestion and metabolism. It produces enzymes to help in the digestion of food, bicarbonates that neutralise stomach acid, and insulin to control blood sugar levels.
Broadly, there are two types of pancreatic cysts:
- Non Neoplastic cysts — benign lesions on the pancreas
- Neoplastic cysts — neoplastic cysts could possibly be or can become cancerous
Pancreatic cysts vs Pancreatitis
Pancreatic cysts can grow as a result of pancreatitis (inflammation of the pancreas).
What causes Pancreatic Cysts?
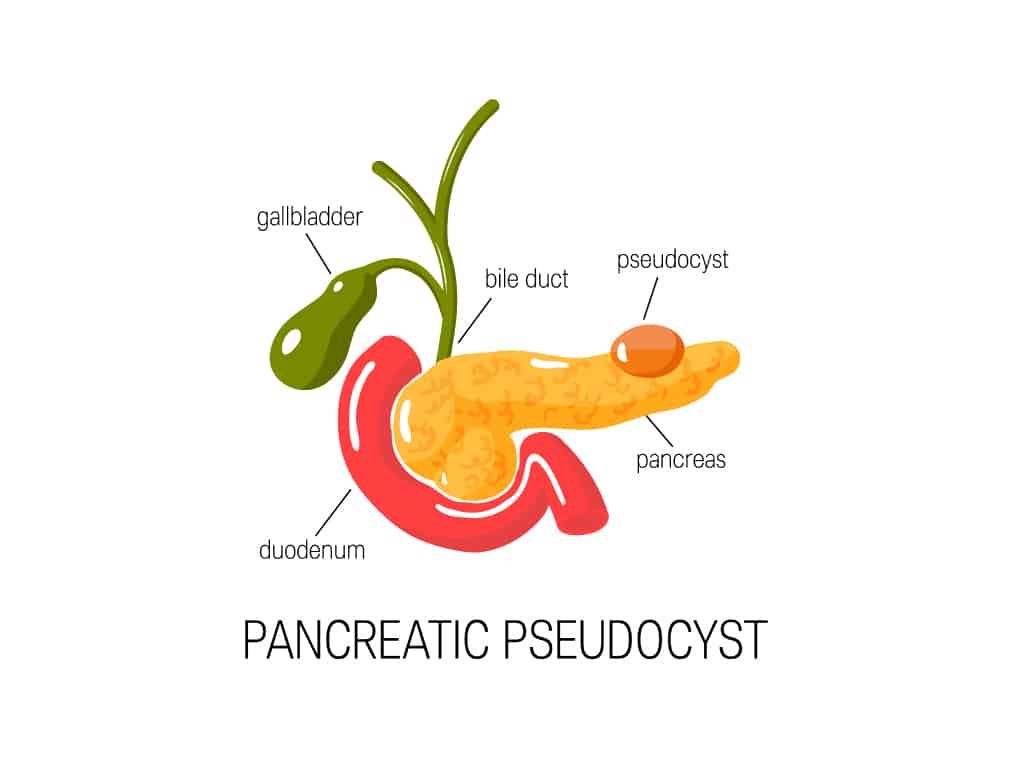
The cause of pancreatic cysts is unclear. Injury to the abdomen and pancreatitis may cause pseudocysts to develop. The risk factors for pancreatic cysts include heavy alcohol consumption, gallstones, and abdominal injury.
What are the Types of Pancreatic Cysts?
There are several types of pancreatic cysts, and the common ones include:
- Pseudocysts — benign and mostly made up of pancreatic inflammatory fluid. They are likely to develop due to a complication from pancreatitis, or inflammation of the pancreas.
- Serous cystadenomas (SCA) — these cysts contain clear fluid and have thick, fibrous walls. They are usually benign and may cause abdominal pain. It occurs most frequently in women over 50 years old.
- Mucinous cystic neoplasms (MCN) — usually located in the body or tail of the pancreas. These cysts have the potential to be cancerous.
- Intraductal papillary mucinous neoplasms (IPMN) — the most common precancerous cysts that grow in the pancreatic ducts. They produce large amounts of fluid that contains pancreatic digestive enzymes. They are commonly found in both men and women over 50 years old and may require surgical removal.
- Solid pseudopapillary neoplasm — rare growths in the body or tail of the pancreas that has both solid and cystic components. These cysts may become cancerous and are commonly found in women younger than 35 years old.
- Cystic neuroendocrine tumour — a type of pancreatic cancer. The tumour is mostly solid, but it can have cyst-like components.
Symptoms of Pancreatic Cysts
Most people with pancreatic cysts do not experience any symptoms. The cysts are usually found due to imaging tests of the abdomen for other medical reasons.
Typical symptoms of pancreatic cysts may include:
- Persistent abdominal pain
- Jaundice
- Nausea and vomiting
- Bloatedness
- Unexplained weight loss
In rare cases, pancreatic cysts may develop serious complications. The cyst can rupture, causing a medical emergency. Cysts that produce mucus-like substances can cause an obstruction in the pancreatic ducts, causing inflammation and infection. In general, seek medical help if you are experiencing symptoms of severe complications such as:
- Severe abdominal pain
- Rapid heart rate
- Fainting or decreased consciousness
- Weight loss
How is a Pancreatic Cysts diagnosed?
Pancreatic cysts are usually found during abdominal scans for other medical problems. Your gastroenterologist may order the following tests to help with the diagnosis of pancreatic cysts:
Blood Tests
Blood tests and tumour markers help test for the possible presence of pancreatic cancer.
- CA19-9 — measures the amount of CA19-9 protein in the blood or cyst fluid. In precancerous cysts, the amount of CA19-9 is elevated.
- Carcinoembryonic Antigen (CEA) — measures the amount of CEA in the blood or cyst fluid taken during an endoscopic ultrasound.
- Liver function — measures the amount of bilirubin which is a waste product created by the liver. Elevated levels of bilirubin could mean a cyst or tumour blocking the bile duct.
Imaging Tests
- Computerised Tomography (CT) scan — provides structural images that help evaluate the size, location, and structure of the pancreatic cyst.
- Magnetic Resonance Imaging (MRI) — provides details on the size and structure of the pancreatic cysts.
- Endoscopic Ultrasound (EUS) — detailed images are taken to look for abnormalities such as a pancreatic cyst. A biopsy may also be conducted during the procedure to take a sample of pancreatic cyst tissue for further analysis.
- Magnetic Resonance Cholangiopancreatography (MRCP) — can help monitor a pancreatic cyst, especially in the pancreatic duct.
A note from Dr Benjamn Yip: Abdominal imaging tests are increasingly done nowadays, and many pancreatic cysts are picked up this way incidentally. As some of these cysts have malignant potential, it is prudent to consult your Gastroenterologist when you are found to have such cysts.
How are Pancreatic Cysts Treated?
Pancreatic cysts are common, and they rarely cause any problems. Most of them do not need to be removed or actively treated. However, it is still important to monitor them carefully as the cysts may progress to a point where they need to be surgically removed. Treatment may also vary according to the characteristics of the cysts.
Surveillance
A benign pseudocyst can be left alone as it rarely causes any symptoms or becomes cancerous. However, some cysts should be monitored.
Drainage
When complications emerge or when symptoms of pancreatic cysts become persistent, the doctor will consider cyst drainage. There are various methods for cyst drainage:
- Endoscopic ultrasound drainage — an echoendoscope is used to drain the cysts. It is less invasive and has a high long-term success rate.
- Percutaneous catheter drainage — a catheter, which is a soft hollow tube, is inserted into the body to remove the cyst fluid.
- Surgical drainage — the procedure is done via open surgery or laparoscopic surgery.
Surgery
Surgery is performed with the primary goal of preserving digestive function. Pancreatic cysts with a risk of cancer and enlarged symptomatic pseudocysts may require surgical removal.
Your Gastroenterologist may recommend surgery for several reasons, such as:
- Size of the cyst larger than 3cm
- The cyst has a solid component
- The pancreatic duct is widened or dilated
- Abdominal pain
Surgical techniques for the removal of pancreatic cysts include:
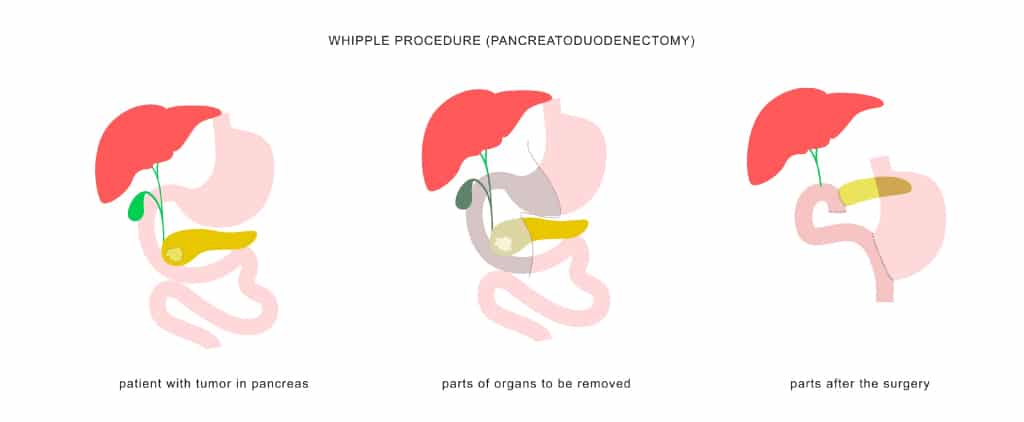
- Whipple procedure — Also known as pancreatoduodenectomy, the procedure removes cysts in the head of the pancreas. During the process, the head of the pancreas, a small part of the intestine, the lower half of the bile duct, surrounding lymph nodes, and the gallbladder are removed.
- Distal pancreatectomy — The procedure removes cysts that are located in the body or tail of the pancreas. During the process, the body and tail of the pancreas and, in most cases, the spleen is removed.
- Total pancreatectomy — When the cysts have affected many parts of the pancreas, the doctor may remove the whole pancreas. Unfortunately, after the procedure, the patient will be life-long dependent on exogenous insulin and pancreatic enzymes.
Summary
One in 40 people have a pancreatic cyst by the age of 40 and generally do not cause any symptoms. However, they could be malignant or ruptured, resulting in a medical emergency. If you do experience the aforementioned symptoms, please consult a gastroenterologist for a proper diagnosis and treatment plan.
References
- Frothingham, S. (2019, January 16). Pancreatic cysts: Symptoms, types, treatment, and risk factors. Healthline. Retrieved from https://www.healthline.com/health/cyst-on-pancreas
- Nassour, I., & Choti, M. A. (2016). Types of pancreatic cysts. JAMA, 316(11), 1226. https://doi.org/10.1001/jama.2016.9035
- Mayo Foundation for Medical Education and Research. (2022, March 5). Pancreatic cysts. Mayo Clinic. Retrieved May 16, 2022, from https://www.mayoclinic.org/diseases-conditions/pancreatic-cysts/diagnosis-treatment/drc-20375997
- Surgery for pancreatic cysts. Memorial Sloan Kettering Cancer Center. (n.d.). Retrieved from https://www.mskcc.org/cancer-care/types/pancreatic-cysts/treatment/surgery-pancreatic-cysts
- Pancreatic cysts and pseudocysts: Symptoms & treatment. Cleveland Clinic. (n.d.). Retrieved from https://my.clevelandclinic.org/health/diseases/14627-pancreatic-cysts-and-pseudocysts
- Watson, K. (2019, March 8). Pancreatitis diet: Foods to eat and avoid. Healthline. Retrieved from https://www.healthline.com/health/pancreatitis-diet#foods-to-eat

