What is Peptic Ulcer Disease?
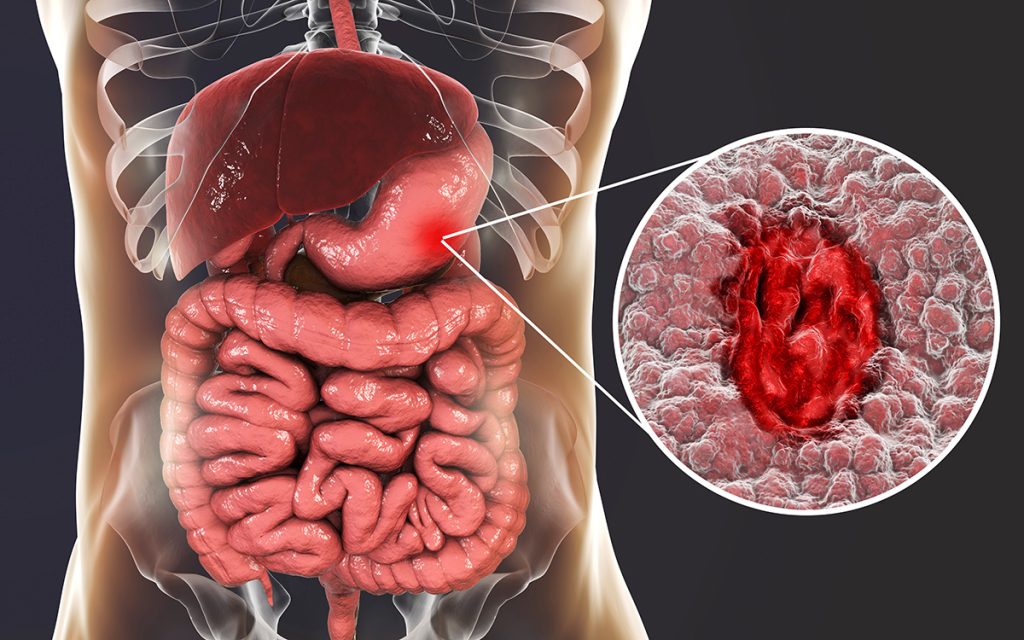
Peptic ulcer disease is a common condition in Singapore where open sores develop in the lining of the stomach (gastric ulcer) and upper portion of the small intestine (duodenal ulcer). According to a study done in 2019, the age-standardised global prevalence rate of peptic ulcer disease is approximately 99.4 per 100,000 population.
Although the disease can affect anyone and at any age, it has been shown that the age-standardised rate for prevalence, incidence, and deaths was higher in males than females over 29 years. One of the main causes of peptic ulcer disease is Helicobacter pylori (H. pylori) infection which affects about 50% of the world’s population. In Singapore, the seroprevalence which is the level of a pathogen in the population, is 31%.
What is the Difference Between Peptic Ulcer Disease and Gastritis?
Patients with peptic ulcer disease share a number of similar symptoms of gastritis, such as upper abdominal pain, nausea, and vomiting, and it must be considered and ruled out when evaluating a patient with suspected peptic ulcer disease.
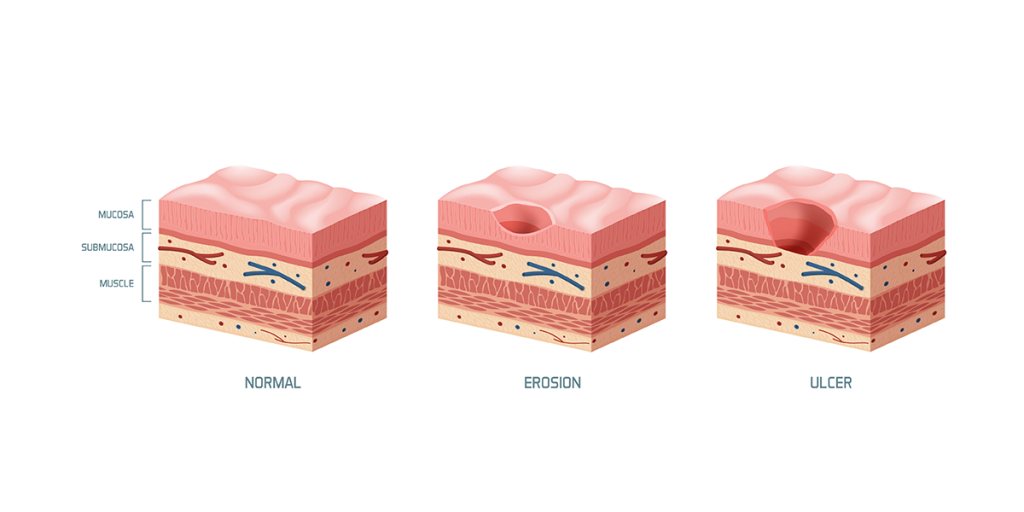
Gastritis refers to a group of conditions that cause inflammation in the lining of the stomach (gastric mucosa), whereas peptic ulcer disease is characterised by the development of open sores in the lining of the stomach or duodenum (proximal part of the small intestine).
Although both conditions cause inflammation in the stomach lining, gastritis indicates general inflammation, while a peptic ulcer is a patch of inflamed stomach lining.
What are the Risk Factors for Developing Peptic Ulcer Disease?
- Smoking
- Chewing tobacco
- Alcohol
- Family history of ulcers
- Kidney, liver, or lung disease
- Frequent use of nonsteroidal anti-inflammatory drugs (NSAIDs)
- On radiation treatments
What are the symptoms of Peptic Ulcer Disease?

The majority of patients do not show or notice any symptoms, but those that do often present with intermittent epigastric pain (upper abdominal pain) and indigestion.
The pain may worsen with an empty stomach and can be relieved temporarily after consuming food or by taking medication to buffer the stomach acid. Do seek medical help if you experience any of the following symptoms, which may indicate a diagnosis of peptic ulcer disease.
Common symptoms that may occur in some patients include:
- Bloatedness
- Burping or belching
- Nausea
- Loss of appetite
- Early satiety (feeling full)
Less common severe symptoms include:
- Vomiting
- Blood in stools or dark stools
- Severe abdominal pain
- Unexplained weight loss
- Intolerance of spicy and fatty foods
What causes Peptic Ulcer Disease?
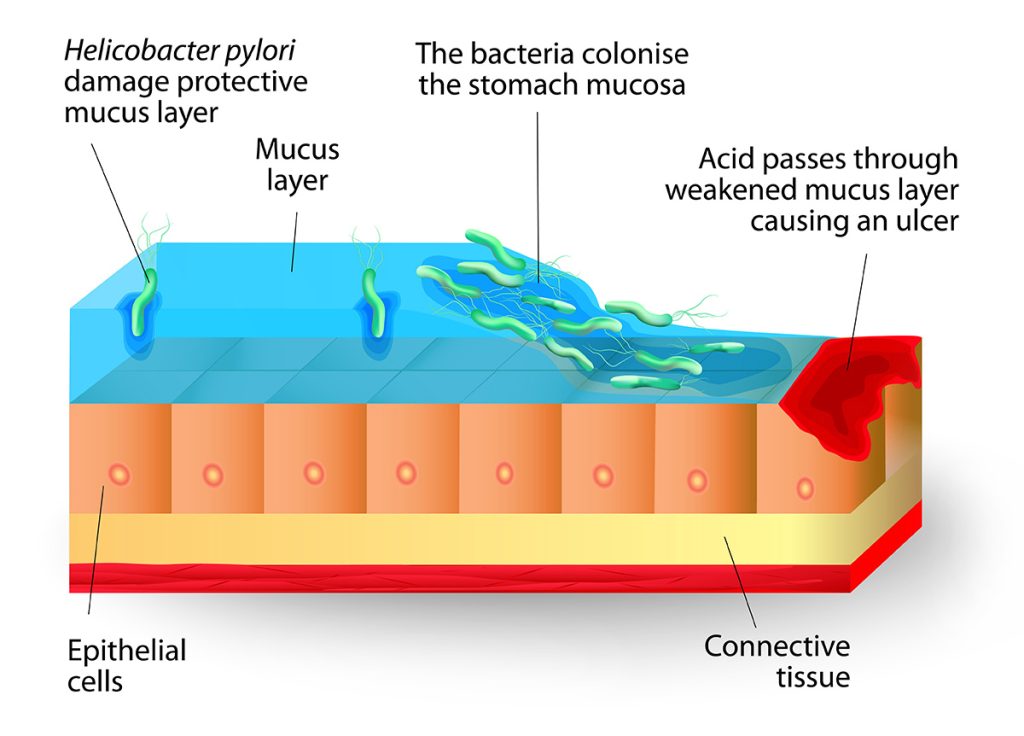
The stomach and small intestine are lined with a mucous layer that protects them against digestive acid (gastric acid). However, an increased amount of acid or decreased amount of mucus may allow the stomach acid to damage the tissue, causing painful open sores to develop.
The predominant causes of peptic ulcer disease are H. pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs), which account for 48% and 24% of cases in the United States. According to a single centre prospective study conducted among 74 patients in Singapore General Hospital (SGH), around 31.73% of patients with peptic ulcer disease were found to be H. pylori positive, while 24.04% were NSAID-related.
H. pylori infection
H. pylori bacteria are commonly present in the mucous layer of the stomach and small intestine. It is often present without symptoms and does not cause any problems. However, H. pylori bacteria can stick to the mucus and cause inflammation, resulting in the breakdown of the mucous layer. Only about 10 to 15% of patients with H. pylori infection eventually develop peptic ulcer disease.
Long term use of NSAIDs
NSAIDs (nonsteroidal anti-inflammatory drugs) are a group of medications often prescribed to relieve pain. However, overuse of these drugs can cause erosion of the mucous layer in the digestive tract, resulting in the development of ulcers. In addition, NSAIDs inhibit cyclooxygenase, which is essential in prostaglandin formation as they have a protective effect on the mucosal lining of the stomach. Common NSAID medications include aspirin, naproxen, and ibuprofen.
Rare causes
Other rare causes that have the potential to cause peptic ulcer disease include being seriously ill from other infections, undergoing surgery, and the intake of steroids.
What Foods Do I Need to Eat or Avoid if I Have Peptic Ulcer Disease?
Contrary to popular belief, stress and spicy food do not cause peptic ulcer disease, although they may exacerbate the condition, making it harder to treat. In general, food rich in antioxidants may be beneficial in activating the immune system to fight the infection and lower your risk of stomach cancer.
Although there is no conclusive evidence to support that a diet free from spicy foods can speed up the healing process or prevent ulcers from recurring there are certain foods that you can include/eliminate from your daily diet to alleviate your symptoms.
Food that may be beneficial:
- Cauliflower
- Blueberries
- Cherries
- Bell peppers
- Leafy vegetables such as kale
- Fermented probiotic food such as miso
- Olive oil
- Turmeric
Food to avoid when you have peptic ulcer disease or acid reflux:
- Coffee
- Chocolate
- Spicy food
- Alcohol
- Acidic food such as citrus fruits
How is Peptic Ulcer Disease diagnosed?

In order to detect a peptic ulcer, your Gastroenterologist may choose to order the following tests:
Laboratory tests
As H. pylori is the most common cause of peptic ulcer disease, blood, stool, or urea breath tests may be carried out to confirm the presence of the infection. In the breath test, you will be asked to consume something that contains radioactive carbon, which will be broken down into carbon dioxide by the bacteria in your stomach. You will then be asked to blow into a bag, and the breath sample will be tested for carbon dioxide. A breath sample will also be taken at the start of the test so that it can be used as a baseline level for comparison. If the level of carbon dioxide has increased in the second sample, it would indicate the patient is H. pylori positive.
Upper gastrointestinal endoscopy
An endoscopy is a non-surgical procedure used to examine and inspect the upper gastrointestinal tract for any abnormalities, such as peptic ulcers. It involves the insertion of an endoscope (a long flexible tube equipped with a light and camera at one end) into the mouth which is passed along the oesophagus, stomach, and small intestine. A biopsy (removal of a tissue sample) of the ulcer may also be obtained for further examination in the lab.
Barium meal
During this procedure, a series of X-ray images of the upper gastrointestinal tract are taken while a white liquid containing barium is swallowed. The barium helps to coat the digestive tract thus giving a clearer visualisation of the peptic ulcer.
Can Peptic Ulcer Disease be cured?
Most cases of peptic ulcer disease can be cured completely by treating their underlying cause, such as eradicating the H. pylori infection or avoiding the usage of NSAIDs. However, peptic ulcers can recur if H. pylori is not completely eliminated from the gastrointestinal tract or if the patient does not stop smoking or taking NSAIDs.
Peptic ulcers can be prevented by protecting yourself from H. pylori infection. Although it is unclear how the bacteria spreads, it is believed to be transmitted from person to person or through contaminated food and water. Hence, it is important to wash your hands frequently and avoid food that is not cooked completely. You can also reduce the risk of peptic ulcer disease by taking caution with the intake of NSAIDs. Try starting with the lowest dose possible (under the guidance of your doctor) and taking the medication with meals.
A note from Alpha Digestive & Liver Centre’s experienced Consultant Gastroenterologist, Dr Benjamin Yip: Non-healing gastric ulcers deserve special attention and follow-ups as they may be the presenting sign of gastric cancers. Hence, if you are diagnosed with a gastric ulcer, he advises patients to undergo a second endoscopy to ensure their gastric ulcer has healed.
How is Peptic Ulcer Disease Treated?
Although peptic ulcers can sometimes heal on their own, they should not be ignored. Without proper and prompt treatment, peptic ulcers can lead to complications such as bleeding, gastric outlet obstruction, and perforation (tearing or rupture).
Peptic ulcers are treated according to the cause. Generally, treatment will involve eliminating the H. pylori bacteria and reducing the use of NSAIDs and other medications to help the ulcer heal. For bleeding ulcers, your Gastroenterologist may choose to treat the ulcers by administering injections through an endoscopy and using a clamp or cauterisation (treatment with heat or a special chemical) to stop the bleeding.
Medications for peptic ulcer include:
- Antibiotics — You may be prescribed antibiotics such as amoxicillin, clarithromycin, metronidazole, and tinidazole to kill the H. pylori bacteria.
- Medications that reduce acid production — Proton pump inhibitors (PPIs) help reduce stomach acid by inhibiting the action of the parts of the cells that produce acid. Histamine blockers, or antihistamines, work by reducing the amount of stomach acid released into the gastrointestinal tract to relieve ulcer pain.
- Antacids — These are medications that neutralise the existing stomach acid, alleviating symptoms such as pain, heartburn, and indigestion.
- Mucosal protective agents — Your Gastroenterologist may also prescribe cytoprotective agents to protect tissues that line the stomach and small intestine.
Medications are typically effective in treating peptic ulcers and will heal the ulcers. However, if symptoms persist despite treatment, another endoscopy may be recommended to rule out other causes. Several reasons, such as non-compliance to medications, antibiotic resistance, and regular use of tobacco and NSAIDs, may keep the ulcer from healing properly.
Refractory peptic ulcer disease is a condition that fails to heal after 8 to 12 weeks of therapy. Therapy options for refractory ulcers involve the treatment of their underlying causes, prolonged administration of PPI, and surgery. Refractory ulcers may be due to other underlying medical conditions such as:
- Zollinger-Ellison syndrome
- Stomach cancer
- Crohn’s disease
- Infection from other bacteria other than H. pylori
What complications can occur when Peptic Ulcer Disease is left untreated?

Untreated peptic ulcers can lead to several health complications such as:
- Bleeding — Upper gastrointestinal bleeding occurs in 15 to 20% of patients with peptic ulcer disease. Peptic ulcers can result in blood loss that leads to anaemia. Severe blood loss may cause bloody stools or vomit.
- Perforation — This occurs in 2 to 10% of patients with peptic ulcer disease. Peptic ulcers can perforate (rupture) the walls of the stomach and small intestine, resulting in serious infection of the abdominal cavity. Chemical and bacterial peritonitis due to peritoneal perforation is a surgical emergency that causes sudden and severe upper abdominal pain.
- Obstruction — Gastric outlet obstruction occurs in less than 5 to 8% of patients with peptic ulcer disease. Recurrent peptic ulcers may lead to the development of pyloric stenosis as a result of inflammation and scarring.
- Gastric cancer — Patients with helicobacter pylori infection have an increased risk of gastric cancer.
Rarely, gallstones (sometimes also known as liver stones) and bile duct stones can result in the inflammation of pancreatitis (inflammation of the pancreas). This could potentially lead to gastric ulcers or worsen pre-existing peptic ulcers.
Summary
Peptic ulcer disease is a common condition of the gastrointestinal tract characterised by the development of peptic ulcers due to the discontinuation of the mucous layer that lines and protects the stomach and small intestine.
As peptic ulcer disease is mainly caused by H. pylori bacteria and the use of NSAIDs, treatment generally involves medication and refraining from NSAID use. If you suffer from peptic ulcer disease or if your symptoms persist even after treatment, do reach out to our team at Alpha Digestive & Liver Centre to schedule a consultation with our experienced Consultant Gastroenterologist and Hepatologist, Dr Benjamin Yip, for further assessment and the proper treatment.
References
- Xie, X., Ren, K., Zhou, Z., Dang, C., & Zhang, H. (2022). The global, regional and national burden of peptic ulcer disease from 1990 to 2019: A population-based study. BMC Gastroenterology, 22(1). https://doi.org/10.1186/s12876-022-02130-2
- Chew, C. A., Lye, T. F., Ang, D., & Ang, T. L. (2017). The diagnosis and management of H. pylori infection in Singapore. Singapore Medical Journal, 58(5), 234–240. https://doi.org/10.11622/smedj.2017037
- Mayo Foundation for Medical Education and Research. (2020, August 6). Peptic ulcer. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/symptoms-causes/syc-20354223
- Peptic ulcer disease: Treatment, symptoms, causes, prevention. Cleveland Clinic. (n.d.). Retrieved from https://my.clevelandclinic.org/health/diseases/10350-peptic-ulcer-disease
- Ramakrishnan, K., & Salinas, R. C. (2007). Peptic Ulcer Disease. Am Fam Physician, 76, 1005–1012.
- Watson, K. (2020, August 21). Stomach ulcer diet: Foods to eat and foods to avoid. Healthline. Retrieved from https://www.healthline.com/health/stomach-ulcer-diet#what-to-eat
- Malik, T. F., Gnanapandithan, K., & Singh, K. (2021, July 29). Peptic ulcer disease. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK534792/
- Peptic Ulcer Disease. Penn Medicine. Retrieved from https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/peptic-ulcer-disease

