What is Gastritis / Duodenitis?
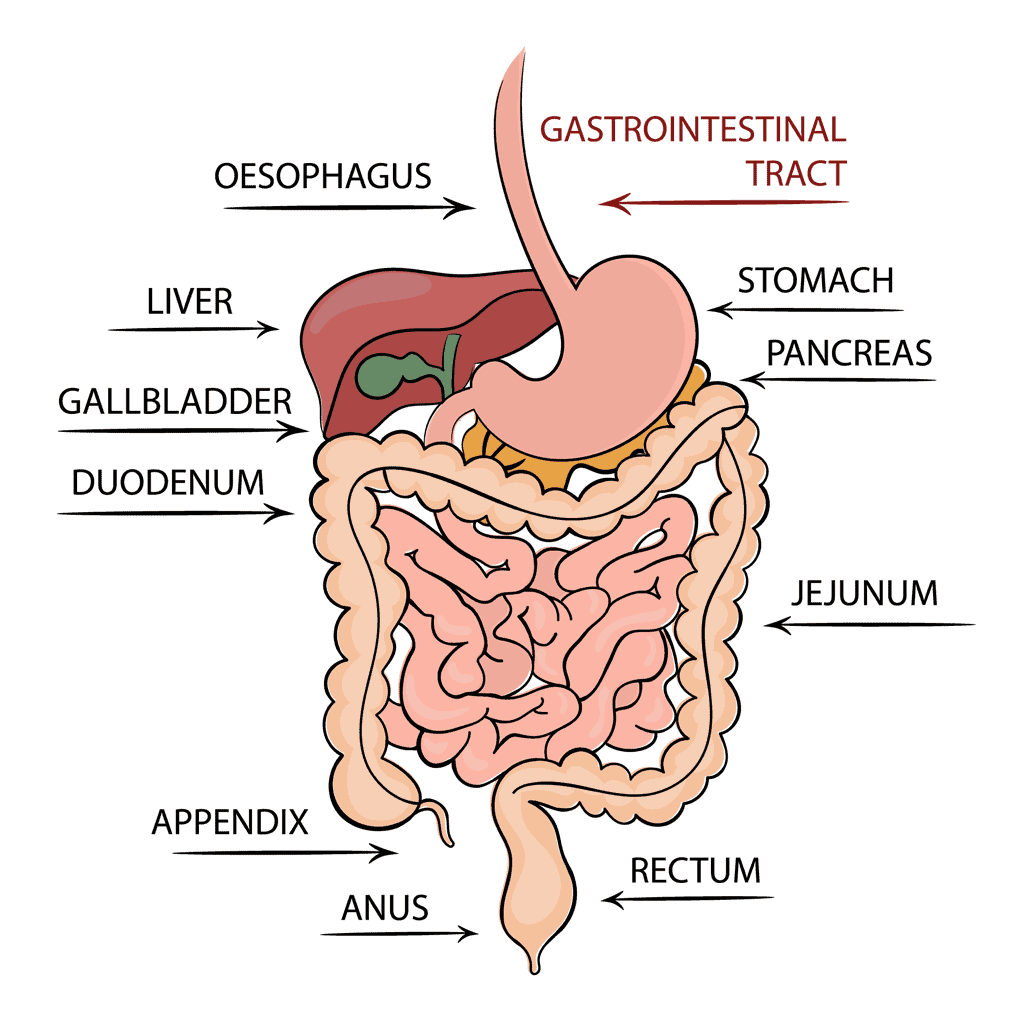
Gastritis and duodenitis, two commonly occurring inflammatory conditions in Singapore, affect different parts of the lining of your gastrointestinal tract. Gastritis involves the lining of the stomach, whereas duodenitis affects the upper part of the small intestine. The duodenum is the most proximal segment of the small intestine and plays a vital role in mixing food with enzymes and bile, aiding digestion.
These conditions can occur in anyone and any age, and may be either acute or chronic. Gastritis and duodenitis generally do not cause serious side effects and are curable with lifestyle changes and medications.
Symptoms of Gastritis / Duodenitis
When people complain of having ‘gastric’ (tummy pain) after skipping lunch, it’s most likely a manifestation of gastritis. Most have mild symptoms that are well-managed with antacids and eating regular meals. Some people do not have any symptoms, and may not even realise they have gastritis/duodenitis.
Common symptoms (if any), include:
- Early satiety (feeling full soon after eating)
- A burning sensation in the stomach
- Abdominal cramps
- Pain
- Indigestion
- Nausea/vomiting
Causes of Gastritis / Duodenitis
The most common cause of both these conditions is H. pylori (Helicobacter pylori), which is a bacterium that can cause infections in the stomach and small intestine. Although it is considered part of the normal flora of the oral cavity and stomach, it can easily colonise your gut and increase your risk of developing gastritis or duodenitis.
H. pylori bacteria are usually passed through direct contact with saliva or other bodily fluids, but they can also be spread through contaminated food and water or even from sharing utensils with infected individuals. Those who live in crowded and unsanitary living conditions and do not have access to a supply of clean water may be at a higher risk of developing H. pylori infection.
Furthermore, this infection can even be transmitted from individuals who harbour the bacteria without showing any symptoms, who themselves may be unaware they are H. pylori carriers.
Some other non-bacterial causes of gastritis/duodenitis include:
- Long-term consumption of aspirin, NSAIDs (ibuprofen, naproxen)
- Excessive alcohol consumption
- Stress
- Cigarette smoking
Although avoiding the causes mentioned above will not completely eliminate the risk of developing these conditions, they can reduce it.
How is Gastritis / Duodenitis diagnosed?
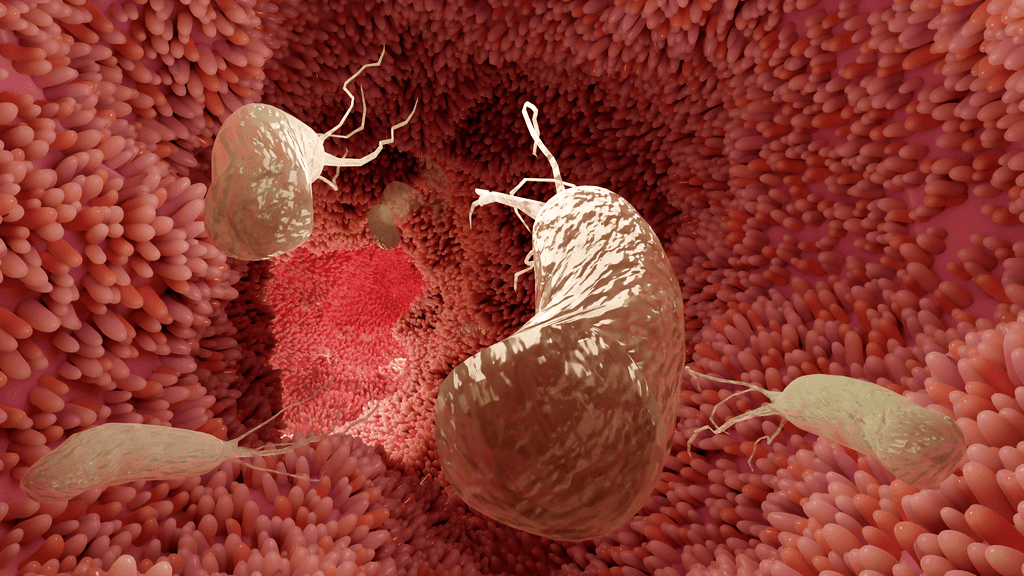
Since both these conditions are most often caused by H. pylori, a simple H. pylori breath test, known as a urea breath test, is carried out to determine if you have the infection or not and to confirm the diagnosis of the infection. This test can also be used to check if the treatment given has cured the infection.
While these bacteria live in the gut, they produce an enzyme called urease, which breaks down urea into ammonia and carbon dioxide. The urea breath test is based on the natural behaviour of the H. pylori bacteria.
You will initially be asked to exhale into a bag, and the amount of carbon dioxide exhaled will be measured and used as a baseline for comparison. Following this, you will be given a liquid containing urea, and after about fifteen minutes of drinking it, you will be asked to exhale into a bag again. The amount of carbon dioxide measured after drinking the liquid will be compared to the initial value. If the second sample has more carbon dioxide than the first sample, you are considered H. pylori positive.
A gastroscopy may also be offered, and it involves inserting a flexible, thin tube down your throat, with a camera attached to the end. This enables your doctor to visualise the appearance of your upper gastrointestinal tract (including the stomach and duodenum) and take samples of your tissue if required. Any inflammation, bleeding, or abnormal masses suggestive of an alternative diagnosis can be visualised, and biopsies (tissue samples) sent for testing if needed.
How is Gastritis / Duodenitis Treated?
Treatment for gastritis and duodenitis depends on the cause, and they typically resolve without any complications.
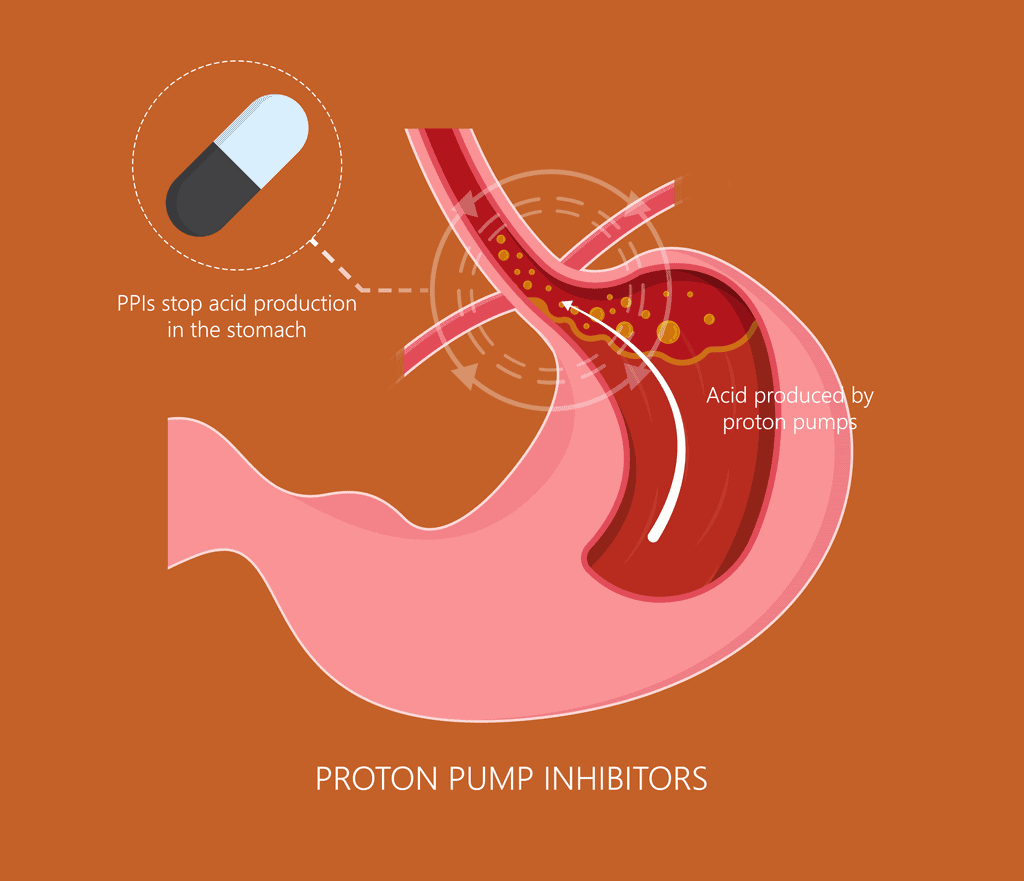
If H. pylori is the cause of your condition, the treatment will aim to eradicate the bacteria through triple therapy. This is a simple medication regimen involving the administration of a proton pump inhibitor (PPI), along with two antibiotics for 14 days. While omeprazole is frequently given, other PPIs may also be used and due to increasing antibiotic resistance, alternative medications may be given. This will be discussed with you during your consultation.
As for other causes of gastritis/duodenitis, treatment includes stopping or reducing the intake of NSAIDs and alcohol. Smoking cessation and stress reduction will also help alleviate the symptoms of both conditions, as well as improve your overall health.
What Complications Can Arise if Gastritis / Duodenitis is Left Untreated?
If the conditions are not treated or poorly managed, they can become chronic, resulting in various serious consequences, such as:
- Bleeding of the lining/mucosa of the gastrointestinal tract — This may manifest as vomit with the appearance of either fresh blood or coffee grounds (digested blood), or passing blood in your stools (black, foul-smelling stools)
- Fever — Chronic inflammation can trigger your body’s immune response and cause a fever
- Weight loss and/or malnutrition — Chronic inflammation results in poorer digestion of food
- Stomach cancer — Chronic inflammation puts one at a higher risk of stomach or duodenal cancer. An endoscopy may be required to assess for the presence of any malignancy
Patients with gastritis and duodenitis generally respond well to the treatment and lifestyle changes mentioned above. Still, if you have any of the symptoms discussed or are concerned about your risk of developing stomach cancer (especially if you have a family history of this cancer), it is advisable to speak to a Gastroenterologist.
Do I Need to Seek Medical Attention from a Gastroenterologist Right Away?
It is advisable to consult your Gastroenterologist if your symptoms persist for more than two weeks. You need to seek immediate medical attention if you experience the following:
- A fever of 38°C or higher
- Severe abdominal pain
- Black stools
- Coffee ground emesis (vomit that looks like coffee grounds)
A Gastroenterologist is a specialist in digestive disorders, who can provide you with the specialised care that you need.
Is it just Gastritis/Duodenitis?
Conditions like peptic ulcer disease and oesophagitis also affect the gastrointestinal tract and may cause similar symptoms of gastritis/duodenitis. Therefore, further assessment may be required to evaluate this.
Peptic Ulcers vs Gastritis/Duodenitis
Peptic ulcer disease is characterised by the development of open sores (ulcers) in the lining of the digestive tract, and it commonly affects the stomach (gastric or stomach ulcers) and duodenum (duodenal ulcers), accounting for almost 20% and 80% of all peptic ulcers respectively.
Peptic ulcers result from the production of excess stomach acid, which is most often caused by H. pylori infection, and the excessive use of certain medications such as NSAIDs (nonsteroidal anti-inflammatory drugs). Other less common causes of peptic ulcers include severe stress, Crohn’s disease, chemotherapy or radiation therapy, and stomach cancer.
Symptoms of these ulcers are fairly similar to those of gastritis and duodenitis, such as burning gastric pain/cramps, feeling full, bloating or nausea. Additional symptoms more unique to peptic ulcers include intolerance to certain foods and pain related to the timing of food intake. However, most individuals with peptic ulcers are often asymptomatic (experiencing no symptoms).
Proton pump inhibitors (PPI) are the first-line treatment for peptic ulcers. They are often prescribed for a few weeks and work by decreasing acidity, allowing the ulcers to have sufficient time to heal and relieve symptoms. Just like gastritis/duodenitis, the treatment for peptic ulcers caused by H. pylori involves eradicating the bacteria using triple therapy.
Oesophagitis vs Gastritis/Duodenitis
As the name suggests, oesophagitis is a condition in which the oesophagus (food tube) is inflamed. It comprises various inflammatory disorders with various causes, such as gastric reflux or eosinophilic, to name a few.
The main difference between oesophagitis and gastritis/duodenitis is simply the site of inflammation - the oesophagus is a part of the gastrointestinal tract directly above and connected to the stomach. The treatment for the various types of oesophagitis depends on the cause, which your doctor will advise you on.
What can I eat if I have Gastritis/Duodenitis?
Your symptoms can be worsened by the intake of certain foods or drinks that increase the acidity in your stomach/intestines or directly cause inflammation to their lining.
In general, patients are advised to reduce the intake of, or avoid:
- Spicy foods
- Highly acidic foods such as citrus fruits, tomatoes, and pineapples.
- Fried or fatty foods
- Alcohol and caffeinated drinks
If you enjoy eating the above foods, they do not have to be eliminated from your diet entirely, but should be taken in reduced quantities or stopped if they worsen your symptoms.
On the other hand, some foods can help alleviate the symptoms of gastritis/duodenitis, and these include:
- Low-acid foods
- Non-caffeinated and non-carbonated drinks
- High fibre foods
- Non-alcoholic beverages
Additionally, eating regular, small portions of food while maintaining a healthy, low-stress lifestyle can often stop gastritis/duodenitis from worsening.
Summary
In conclusion, gastritis, duodenitis, and other common inflammatory conditions of the gastrointestinal tract may be caused by a variety of reasons. Fortunately, there are various treatment options, both medical and lifestyle-related.
Alpha Digestive & Liver Centre’s experienced Consultant Gastroenterologist, Dr Benjamin Yip, reminds us that even though gastritis/duodenitis is benign (non-cancerous), their symptoms can be similar to gastric cancer, which is often lethal and can occur in individuals in their 30s or 40s. If in doubt, get in touch with our friendly team today and schedule an appointment to consult Dr Benjamin Yip.
References
- “Helicobacter pylori and Gastric Cancer: Factors That Modulate Disease Risk.” NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2952980/. Accessed 4 October 2022.
- “Helicobacter pylori infection: old and new - PMC.” NCBI, 4 June 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5467250/. Accessed 4 October 2022.
- Kuipers, Ernst J. “PPIs for prevention and treatment of peptic ulcer.” The Lancet: Gastroenterology & Hepatology, https://www.thelancet.com/journals/langas/article/PIIS2468-1253(18)30047-5/fulltext. Accessed 4 october 2022.
- Li, Yan. “What Roles Do Probiotics Play in the Eradication of Helicobacter pylori? Current Knowledge and Ongoing Research.” NCBI, 16 October 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6206577/. Accessed 4 October 2022.
- “Stress-Induced Gastritis - StatPearls.” NCBI, 1 May 2022, https://www.ncbi.nlm.nih.gov/books/NBK499926/. Accessed 4 October 2022.
- “Helicobacter pylori and gastric disease” NIH, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1113159/#:~:text=H%20pylori%20can%20thus%20be,children%20are%20acquiring%20H%20pylori. Accessed 29 February 2024.
- “Helicobacter pylori: A Beneficial Gastric Pathogen? NIH, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4291894/. Accessed 29 February 2024.

