
What is IBS?
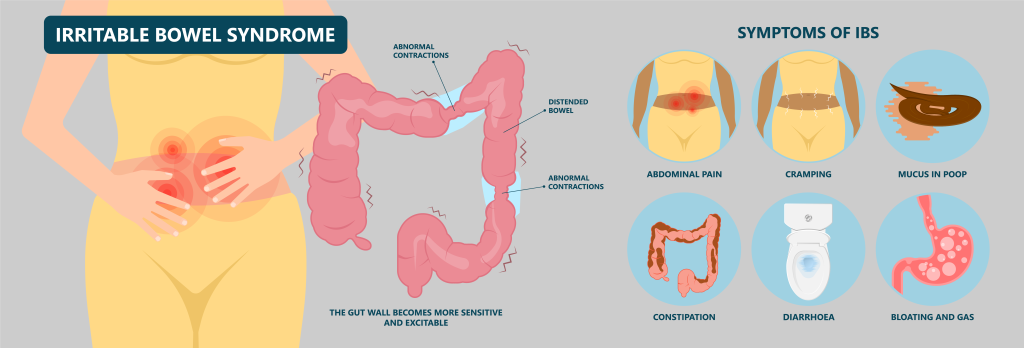
IBS (irritable bowel syndrome), not to be confused with IBD (inflammatory bowel disease), is a common chronic disorder affecting the large intestine, with no known cause. It is a functional disorder manifesting with symptoms such as abdominal cramps or pain, bloating, constipation and/or diarrhoea, but the symptoms may vary depending on the subtype of IBS and its severity.
It is important to note that IBS is a medical diagnosis and not an all-encompassing term your Gastroenterologist uses when they cannot determine the exact cause of your bowel issues. However, because the condition often has no definitive cause, it also does not have a definitive cure.
Treatment largely revolves around minimising and managing IBS symptoms. Most people do not develop severe IBS and are able to cope by managing their diet, lifestyles or stress levels. More severe IBS may be treated with certain medications. If you do experience any irritable bowel syndrome symptoms, it is important to seek medical attention as it may be indicative of a more serious condition.
How common is IBS in Singapore?
Irritable bowel syndrome is a common condition that affects around 10% of the population in Singapore, mostly those in their 30s and 40s. IBS is also more commonly found in women than men, with gastrointestinal experts believing the cause for this is due to the way in which female hormones modulate their brain-gut interactions.
What are the symptoms of IBS?
Irritable bowel syndrome is usually a life-long condition with persistent signs and symptoms. These symptoms can vary from person to person, and one’s pattern of symptoms may even change over time. The most common IBS symptoms are:
- Abdominal cramps, pain or discomfort, often associated with bowel movements
- Increased frequency of bowel movements or flatulence (passing gas)
- Altered appearance of stools (e.g., constipation, diarrhoea, mixed, mucoid)
- Bloating
- Lethargy and fatigue
The list of symptoms, however, is non-exhaustive, and a person living with IBS may have a few or all of these, depending on the severity of their condition.
When are the ‘red flag’ indicators of IBS?
If you are suffering from irritable bowel syndrome, you need to be aware of the following symptoms:
- Age of onset over 60
- Fever and chills
- Anaemia
- Elevated inflammatory markers
- A family history of bowel or ovarian cancer
- Unexplained weight loss
- Abdominal or pelvic masses
- Blood in stools
- Night sweats
Can dairy cause IBS?
Dairy may cause IBS symptoms, especially if the dairy product is high in fat. Switching to low-fat or non-fat dairy products may alleviate your symptoms.
How do I tell the difference between IBS and other diseases?
There are many gastrointestinal diseases that can mimic the symptoms of IBS, including coeliac disease, early inflammatory bowel disease, and even colorectal cancer, and treatment will vary depending on the underlying cause.
How is IBS diagnosed?
It is important to note that IBS is a diagnosis of exclusion. This means that your Gastroenterologist will rule out other possible conditions causing these symptoms before confirming the diagnosis.
The Rome IV criteria is used to diagnose IBS, and the diagnostic criteria are as follows (quoted from the Rome Foundation Website):
- Recurrent abdominal pain, on average at least one day/week in the last three months, is associated with two or more of the following criteria:
- Related to defaecation
- Associated with a change in the frequency of stool
- Associated with a change in form (appearance) of stool
- Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
There is no single diagnostic test for IBS but investigations such as blood, stool, and hydrogen breath tests may be performed to assess your baseline. While these tests are not required to come to a diagnosis, they are beneficial in ruling out more serious conditions.
Colorectal cancer screening may play a vital role in the exclusion of colorectal cancer and other diseases. The most commonly performed screening test for colorectal cancer is a colonoscopy, and it may be carried out as a routine age-based investigation.
Three subtypes of IBS
IBS is often grouped into three broad subtypes to guide treatment, and they are based on the predominant type of stool on days with at least one abnormal bowel movement:
- IBS-C (IBS with constipation)
- IBS-D (IBS with diarrhoea)
- IBS mixed (IBS-M)
If your symptoms do not fall under these three subtypes, it may be classified under the umbrella of IBS-U (IBS Unspecified).
IBS with constipation (IBS-C)
Most of your stools are hard and lumpy.
IBS-C is diagnosed if constipation is the predominant type of stool on ≥25% of the days when you have at least one abnormal bowel movement, and ≤25% of the days are characterised by diarrhoea. When a patient is constipated, his or her stools often appear lumpy, and sausage-shaped or like hard pellets.
Patients with this chronic condition often experience constipation, less frequent bowel movements, abdominal pain and bloating. However, constipation can lead to straining when defecating, and you may notice some blood when wiping afterwards.
IBS with diarrhoea (IBS-D)
Most of your stools are loose and watery.
IBS-D is the opposite of IBS-C: it is diagnosed when diarrhoea is the predominant type of stool on ≥25% of the days when you have at least one abnormal bowel movement and ≤25% of the days are characterised by constipation.
This subtype is often associated with increased frequency of bowel movements, cramp-like abdominal pain (related to defecation), bloating and gas.
IBS-mixed (IBS-M)
Most of your stools are hard and lumpy and loose and watery (on the same day).
This mixed subtype (IBS with mixed bowel habits) is a complex disorder that alternates between constipation and diarrhoea.
In this form of IBS, out of all the days when you have at least one abnormal bowel movement, constipation is the predominant type of stool on ≥25% of the days, and diarrhoea predominates on ≥25% of the other days.
Can IBS be cured and how is it treated?
There is no definitive cure for IBS at the moment, hence treatment revolves around relieving IBS symptoms and minimising the impact of it on patients’ lives.
Patients with milder symptoms can often cope by managing their diet and lifestyle. Certain types of food can aggravate or increase the frequency of bowel movements and should be avoided.
Leading a healthy lifestyle, in general, helps as well, and this includes managing stress levels, having adequate hydration and a high-fibre diet and regular exercise.
For those with more severe symptoms or if IBS is significantly hampering their daily life, your Gastroenterologist may prescribe medication to ease the symptoms. Various medications may be prescribed to mildly alleviate abdominal cramps and reduce the frequency of diarrhoea. Laxatives may also be provided to relieve constipation. If stress is a significant trigger for IBS, psychological therapy in the form of counselling may be of use as well.

How about the Low-FODMAP diet?
FODMAP refers to fermentable oligosaccharides, disaccharides, monosaccharides and polyols, which are short-chain carbohydrates (sugars) that are often more difficult for the small intestine to absorb.
The Low-FODMAP diet is a temporary restrictive diet that allows the patient to discern what foods may be causing their IBS symptoms. This involves avoiding FODMAP foods and slowly reintroducing them into your diet to see how your digestive system responds.
By understanding exactly what types of food are causing your IBS symptoms, you will be able to effectively manage your IBS while enjoying your worry-free life.
Summary
IBS symptoms are varied and can occur in many other digestive diseases as well. Therefore, it is important for you to be assessed by a Gastroenterologist to ensure that you do not have any serious underlying digestive conditions.
While irritable bowel syndrome is a lifelong condition with no definitive cure, it can be well-controlled if you are compliant with your Gastroenterologist’s treatment plan to minimise the impact IBS has on your daily life.
Get in touch with Alpha Digestive & Liver Centre today and schedule your appointment with our experienced Consultant Gastroenterologist Dr Benjamin Yip for an accurate diagnosis.
References
- Blanton, Nicole. “The gut-brain connection: How psychotherapy treats irritable bowel syndrome.” Baylor College of Medicine Blog Network -, 10 January 2019, https://blogs.bcm.edu/2019/01/10/the-gut-brain-connection-how-psychotherapy-treats-irritable-bowel-syndrome/. Accessed 11 May 2022.
- “Ease IBS Symptoms With a High-Fiber or Low-Fiber Diet.” UPMC HealthBeat, 26 March 2016, https://share.upmc.com/2016/03/ibs-high-fiber-diet/. Accessed 11 May 2022.
- Khatri, Minesh. “Diverticulitis Treatment: How To Treat It & Recovery Time.” WebMD, 21 June 2021, https://www.webmd.com/digestive-disorders/understanding-diverticulitis-treatment. Accessed 11 May 2022.
- “Colorectal Cancer in Inflammatory Bowel Disease.” PubMed, https://pubmed.ncbi.nlm.nih.gov/29720903. Accessed 11 May 2022
- “Rome IV Criteria - Rome Foundation.” The Rome Foundation, https://theromefoundation.org/rome-iv/rome-iv-criteria/. Accessed 11 May 2022.
- NHS. “Irritable Bowel Syndrome”. https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/ Accessed 24 January 2024.
- WebMD. “Irritable Bowel Syndrome”. https://www.webmd.com/ibs/digestive-diseases-irritable-bowel-syndrome Accessed 24 January 2024.
- NUHS. “Irritable Bowel Syndrome”. https://www.nuhs.edu.sg/For-Patients-Visitors/find-a-condition/Pages/Irritable+Bowel+Syndrome.aspx Accessed 25 January 2024.

