What are Bile Duct Strictures?
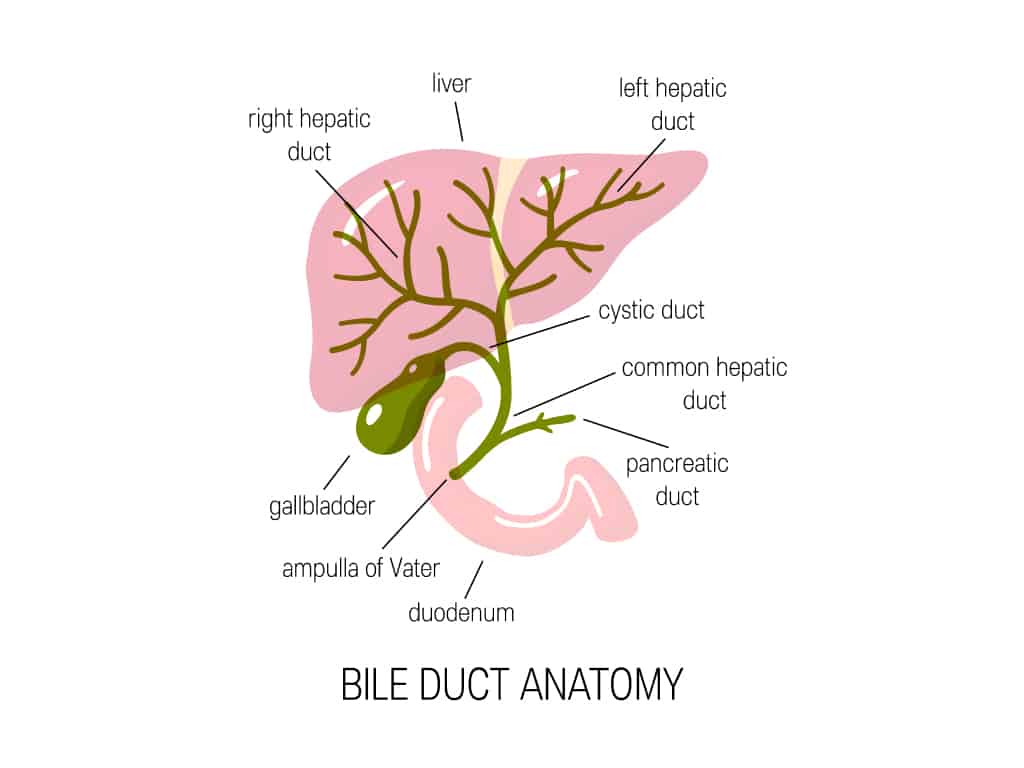
The biliary tract consists of the liver, gallbladder, and bile ducts. There are bile ducts both within (intrahepatic) and outside (extrahepatic) the liver. The term ‘hepatobiliary’ is used to refer to the liver and bile ducts.
The liver produces bile, which aids in the digestion of the fats found in the food we eat by breaking it down into smaller pieces (emulsification). It also helps to clear waste produced by the liver by helping carry waste out of the liver. Bile contains water, bile acids, cholesterol, phospholipids, electrolytes, and a compound known as bilirubin. Some components of bile are made by liver cells, while the rest are extracted from the blood by the liver.
Once bile is produced, it exits the liver and is typically stored in the gallbladder before being released into the common bile duct and subsequently into the duodenum, which is the first part of the small intestine.
As such, bile duct strictures refer to segments of the bile duct that are narrowed. Narrowed segments can be found either within the intrahepatic bile ducts, extrahepatic bile ducts, or the common bile duct. Strictures can be harmful as this narrowing obstructs the flow of bile from the liver into the small intestine, resulting in dilatation of the bile ducts above the narrowed segment and an accumulation of bile above the stricture.
The management of bile duct strictures depends on the cause of the stricture, which can be broadly classified as either benign or malignant. The vast majority of bile duct strictures are malignant (around 70%).
Why are Bile Duct Strictures a problem?
Bile duct strictures are a problem because they cause narrowing within the biliary tract, which can obstruct the flow of bile from the liver into the small intestines. This results in an accumulation of bile and can cause the bile ducts below the strictures to become dilated. This can cause several complications, including:
- An increased risk of infection to the bile ducts (cholangitis)
- Jaundice
- Impaired digestion of food
If left untreated, strictures can also increase the risk of liver damage and liver cirrhosis, where the liver function is impaired and where liver tissue is replaced by scar tissue.
What causes Bile Duct Strictures?
Benign bile duct strictures
Causes of benign bile duct strictures include:
- Damage and scarring due to a gallstone, resulting in a narrowing of the bile duct(s) due to scar tissue build-up
- Damage and scarring after surgery to the biliary tract, including gallbladder removal (cholecystectomy)
- A complication of pancreatitis, which refers to an inflammation of the pancreas (of which there can be multiple causes including gallstones, infections, certain medications like steroids, etc.)
- Primary sclerosing cholangitis, a rare disease that attacks the bile ducts
Malignant bile duct strictures
The two major malignancies causing the strictures are pancreatic adenocarcinoma (a type of pancreatic cancer) and cholangiocarcinoma (gallbladder cancer). Any other type of cancer within the biliary tract are also risk factors for developing malignant bile duct strictures.
What are the symptoms of Bile Duct Strictures?
Symptoms of bile duct strictures include:
- Abdominal pain on the upper right side of the abdomen
- Increased itching over the body (pruritus)
- Fever, chills
- Loss of appetite
- Jaundice (yellowing of eyes and skin, pale or clay-coloured stools, dark brownish-red urine)
- Nausea and vomiting
- Generalised discomfort
How are Bile Duct Strictures diagnosed?
Bile duct strictures are typically diagnosed through imaging studies that allow your Gastroenterologist to visualise the bile duct and biliary tract. Blood tests may also be done to check for enzymes in the liver and biliary tract to determine whether or not the flow of bile has been obstructed and to ascertain the overall function of the liver, including whether or not there is jaundice or damage to liver cells.
Some imaging studies may be ordered, including:
- Ultrasound of the liver: An ultrasound is safe and easy to perform. While it cannot visualise the exact size of the stricture, in most instances it can show changes in the biliary tract that suggest a stricture.
- CT/MRI scans: These scans help in detecting small bile duct strictures, and are precise in visualising the organs in the biliary tract. A chemical called a contrast might be injected into a vein below your skin that will cause the biliary tract to light up on the scan, enabling clearer observation of the biliary tract.
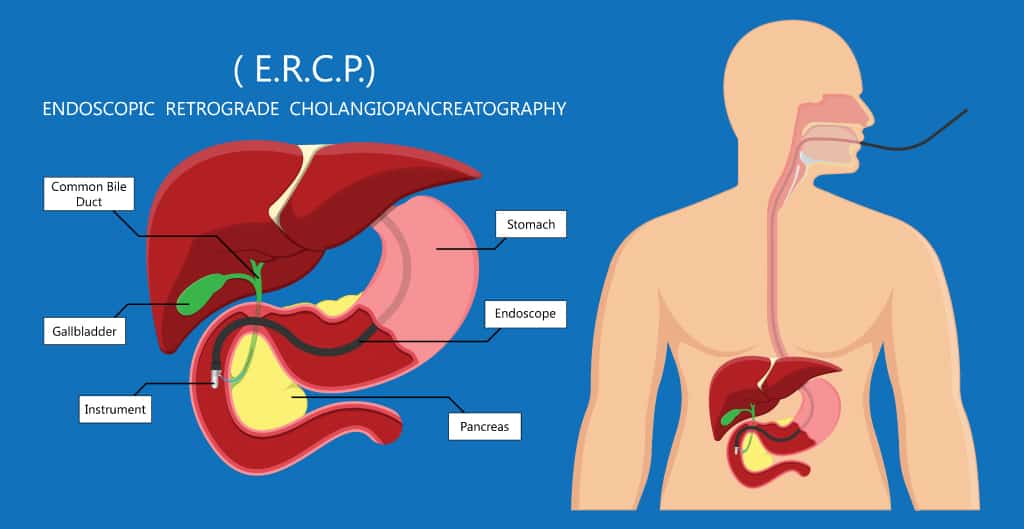
- ERCP (endoscopic retrograde cholangiopancreatography): A long, flexible, hollow tube with a video camera attached to it (endoscopy) is inserted through the mouth and into the biliary tract. ERCP is also therapeutic and can remove stones and manage strictures.
- Some light sedation is given during the procedure to help make patients more comfortable. Once sedated, the scope typically enters through the mouth and into the small intestine and biliary tree.
- Once the Gastroenterologist identifies the area where the bile duct joins the intestines (at the ampulla of Vater), a minute tube called a guide wire will be inserted through the ERCP scope tube. Serial x-rays will be taken once the contrast is inserted, which will enable the Gastroenterologist to visualise the biliary tract as the contrast moves through the bile ducts, gallbladder, and pancreas.
What are the treatments for Bile Duct Strictures?
Often, bile duct strictures are treated either with a procedure or surgery:
Procedures
- Endoscopic Retrograde Cholangiopancreatography (ERCP) can be done to treat the stricture by way of a biliary stent. A stent is a small metal or plastic tube that will be inserted through the ERCP endoscope and used to open up the stricture.
- Percutaneous Transhepatic Cholangiography (PTC) involves the insertion of a catheter (drain) through the skin, on the right side of the abdomen. The catheter helps drain any collections that might be present in the liver (which can consist of accumulated bile) and helps keep the stricture open.
Bile duct strictures often need to be managed with advanced endoscopy techniques, and not all Gastroenterologists are not trained to do these procedures. This makes it important to find one who can perform these procedures effectively.
Surgery
In rare cases, surgery has to be performed for a biliary stricture. The surgeons will resect (i.e. take out) the narrowed part of the bile duct, and the healthy, upper portion will be connected to the small intestine.
How long can the stent last in the bile duct?
The mean duration of the patency of the stent is about 6 months, and studies recommend their replacement after 3-6 months.
What happens when I need to replace the stent?
Biliary stents can be replaced via ERCP.
What food should I avoid with a Bile Duct Stricture?
Overall, there are no restrictions on what you can eat. However, if you have had a previous history of gallstones, it is advisable to avoid fatty, oily food as they may cause abdominal pain and discomfort.
A healthy diet, quitting smoking, and sufficient exercise are advised if you are preparing for a procedure or surgery in order to help optimise your health and reduce any risks of complications thereafter.
Summary
Bile duct strictures can be both due to benign and malignant causes, and it is important to watch out for any warning symptoms that might point to their diagnosis, as a vast majority of these strictures are due to malignancies. Do consult your Gastroenterologist for a detailed diagnosis and personalised treatment plan.

