What is Anaemia?
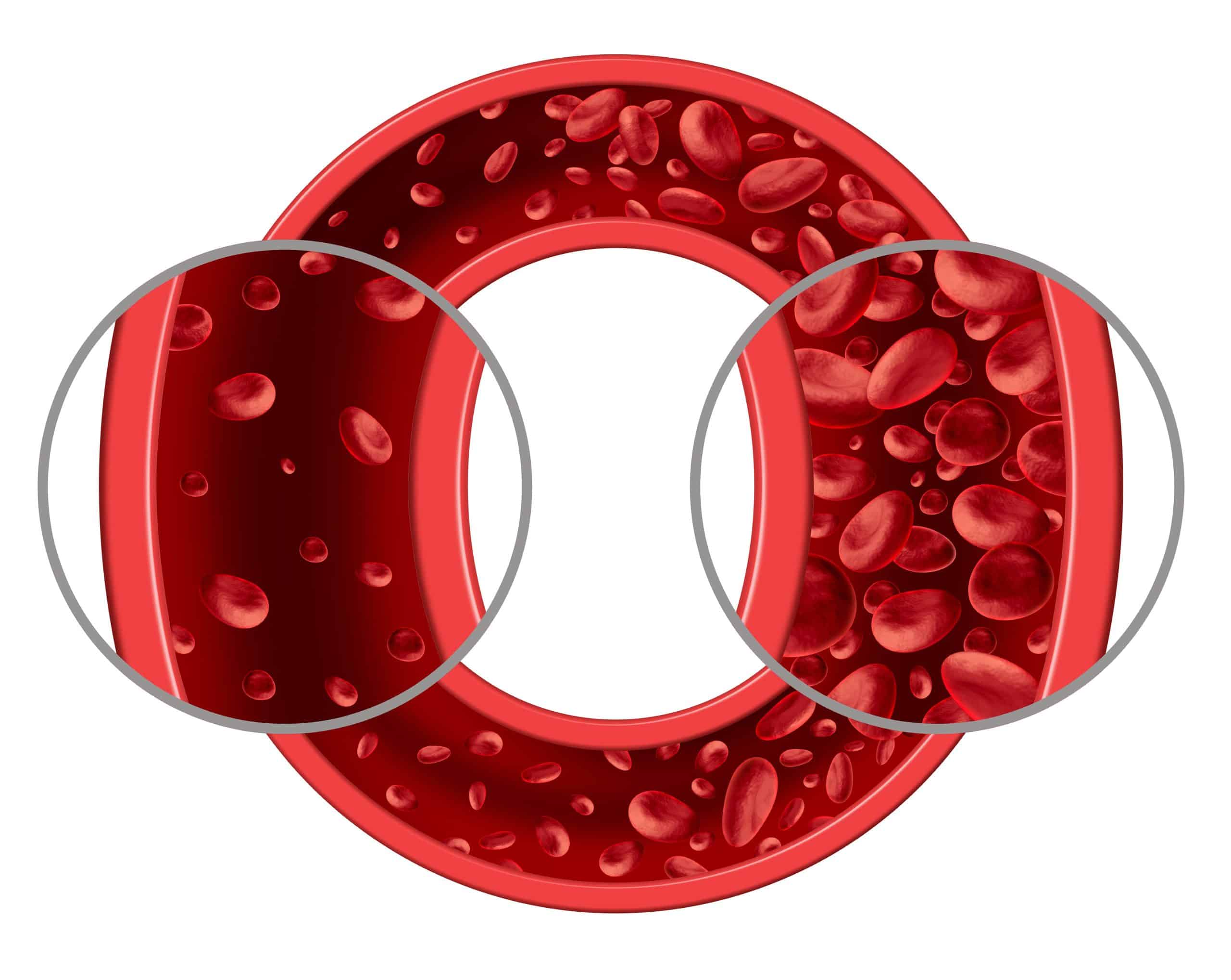
Anaemia is a serious health condition that affects 30% of the world’s population and is also commonly found among individuals in Singapore, especially women. It is caused by an inadequate amount of red blood cells. These cells consist of a protein known as haemoglobin, which carries oxygen through the bloodstream from our lungs to all our tissues and organs, allowing us to go about our daily lives.
There are several types of anaemia, and they can be classified according to their causes. Anaemia can occur suddenly (acute) or result as a consequence of a gradual decline of red blood cells over time (chronic). Anaemia symptoms can range from mild to severe, with some presenting as a warning sign of an underlying disease.
The most common causes of anaemia include:
- Insufficient red blood cells or haemoglobin production (iron deficiency anaemia, thalassemia, chronic infections, bone marrow and stem cell problems, and excessive alcohol intake)
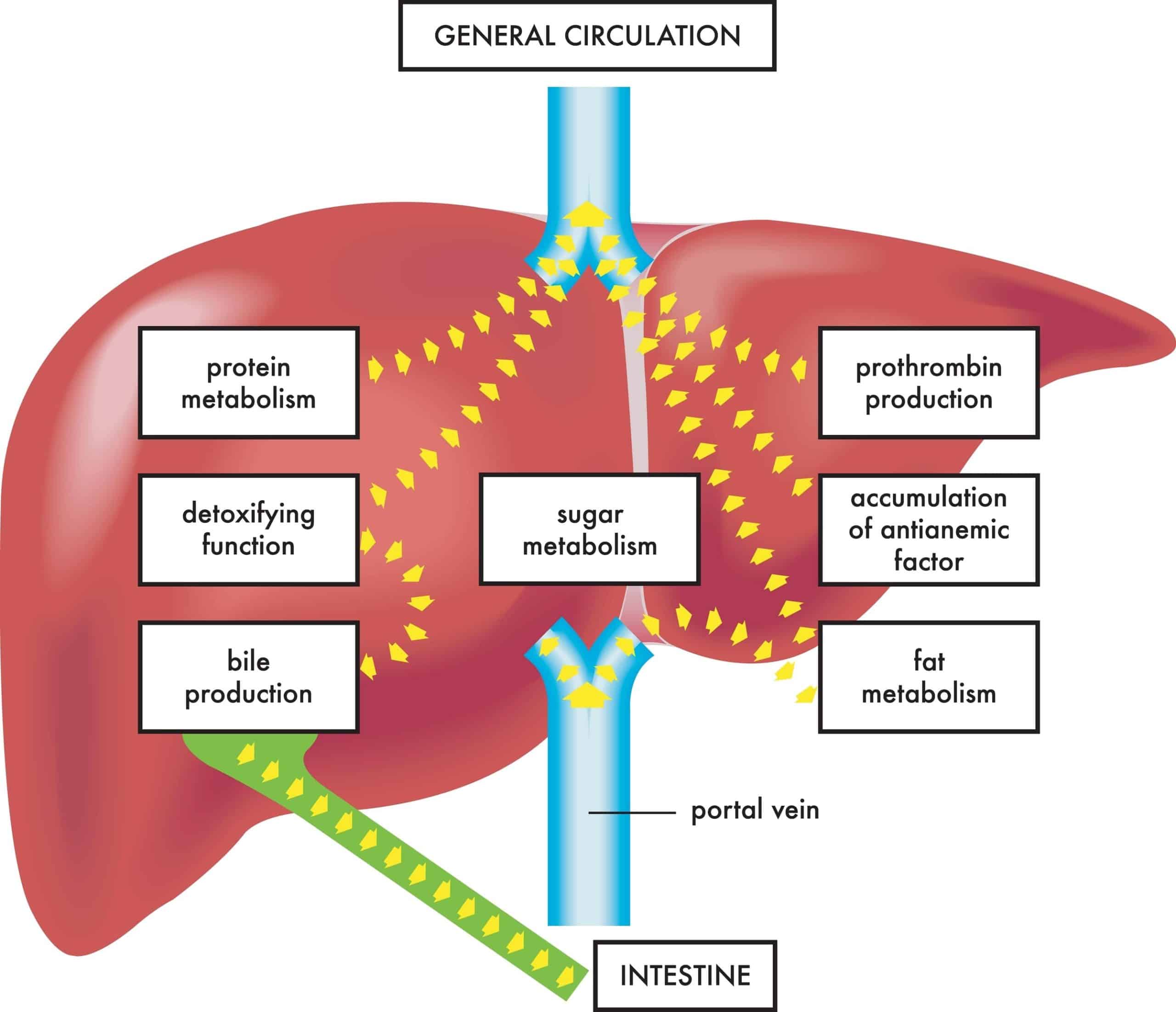
- Increased red blood cell destruction or breakdown (sickle cell anaemia, an enlarged spleen, advanced liver or kidney disease, severe burns, and various haemoglobin disorders)
- Blood loss (post-surgery, certain gastrointestinal conditions like ulcers, haemorrhoids, and cancer, and medications such as NSAIDs)
What is Iron Deficiency Anaemia?
Iron deficiency anaemia is the most common cause of anaemia worldwide. It is caused by insufficient iron stores in the body, leading to the inadequate synthesis of haemoglobin.
Causes of iron deficiency anaemia include:
- Increased blood loss — This can occur as a result of menstruation (especially if the woman has heavy periods) or chronic blood loss due to medical conditions such as ulcers, tumours, polyps, and haemorrhoids.
- Low dietary intake of iron — Picky eaters/children, vegetarians, or people living in less developed countries are at higher risk.
- Iron malabsorption — Those who have digestive conditions like coeliac disease or have undergone any surgical procedures like a gastrectomy (removal of all or part of the stomach) may not be able to absorb sufficient iron from digested food.
- Pregnancy — During pregnancy, the volume of blood increases, and so does the amount of iron. The foetus also uses the mother’s iron supply to synthesise its own haemoglobin. Therefore, if the pregnant woman does not get enough iron or have sufficient iron stores, they can go on to develop iron deficiency anaemia.
Who is at risk of developing Iron Deficiency Anaemia?
Some groups are at a higher risk of developing iron deficiency anaemia:
- Women, especially those with heavy or frequent menstruation or pregnant women not on iron supplementation
- Children who happen to be picky eaters and are not willing to eat iron-rich foods such as green leafy vegetables, meat, eggs
- Vegetarians may be at a higher risk, depending on the type and quantity of vegetables they consume
- Frequent blood donors, since blood donation requires the body to synthesise more red blood cells to replace what was donated
What are the Symptoms of Iron Deficiency Anaemia?
Iron deficiency anaemia can range in severity from patients being completely asymptomatic to having concerning symptoms, such as chest pain.
Common signs and symptoms of iron deficiency anaemia include:
- Weakness
- Fatigue
- Decreased ability to concentrate
- Noticeably pale skin, lips, and eyelids
- Giddiness or lightheadedness
- Decreased ability to exercise
- Headaches
In more severe cases, you may even experience:
- Chest pain, shortness of breath, increased heart rate
- Painful, red, and swollen tongue
- Brittle nails
- Pica (eating disorder) — cravings for ice, paper, soil, or other non-nutritious substances
‘Anaemia eyes’ test
This self-examination can be done in seconds, and all you need is a mirror! You simply pull your lower eyelids down so that the inner layer can be seen in the mirror. In a non-anaemic person, it should be pinkish red, but if you have anaemia, it may appear pale pink or yellowish-white.
Can “anaemia tongue” Point to Iron Deficiency Anaemia?
Anaemia tongue or glossitis is a prominent symptom of iron deficiency anaemia and is characterised by the following:
- Painful, tender and swollen tongue
- Reddish tongue with or without white patches
- Difficulty in speaking, chewing or swallowing
- Smooth appearance of the tongue due to loss of tongue papillae (the small bumps visible on a normal tongue)
How is Iron Deficiency Anaemia Diagnosed?
Iron deficiency anaemia is diagnosed by carrying out a number of blood tests, including a full blood count (FBC) and iron panel. The full blood count, also known as complete blood count (CBC) will measure various cellular components of your blood, such as red blood cells, white blood cells, platelets, haemoglobin, and haematocrit.
If you have iron deficiency anaemia, your blood test results will indicate a low level of iron with a low red blood cell count, and your red blood cells will be smaller and paler than normal. Your blood tests may also show the following:
- Low haematocrit ( percentage of red blood cells)
- Low ferritin (amount of protein that stores blood)
- Low mean cellular volume (average size and volume of red blood cells)
- Low iron saturation (amount of iron in the blood)
- High TIBC (total iron-binding capacity)
Additionally, further tests may be done to identify an underlying cause, such as bleeding from various sites, tumours or ulcers, and they include the following:
An endoscopy may be done. It involves inserting a flexible, thin tube down one’s throat, with a camera attached to the end, enabling direct visualisation of the appearance of your upper gastrointestinal tract (including the stomach & duodenum) and sampling of your tissue if required. Similarly, a colonoscopy may be offered. It involves the insertion of a flexible tube with a camera into the rectum and guided upwards into the colon. Any ulcers, bleeding, or abnormal masses suggestive of an underlying cause can be readily identified.
Endoscopy: This involves inserting a flexible, thin tube down your throat, with a camera attached at one end, enabling direct visualisation of the insides of the upper gastrointestinal tract (including the stomach and duodenum). A tissue sample may also be obtained if needed. Some Gastroenterologists may prefer using an endoscopic ultrasound over the conventional endoscopy because it can enhance the visualisation of the insides of the gastrointestinal tract and its surrounding structures.
Colonoscopy: This involves the insertion of a flexible tube with a camera at one end into the rectum and guided upwards into the colon. Any ulcers, bleeding, or abnormal masses suggestive of an underlying cause can be easily identified through this modality.
Apart from symptoms of iron deficiency anaemia, doctors will also need to know about the kind of medications or supplements you are taking because the iron supplements that are prescribed for the treatment of iron deficiency anaemia can decrease the efficacy of some of your medications.
How Can I Check My Iron Levels at Home?
Conventionally, iron levels are checked during routine visits to the doctor. However, if your doctor advises you to check your levels at home, there are various test kits that allow you to do it yourself at home.
There are various brands on the market, but in general, they involve obtaining a small sample of your blood (using a small lancet included in the kit) and placing it into the test cassette. It is rather similar to checking one’s own blood sugar in diabetic patients, and the cassette resembles COVID self-test kits.
The results of the test should always be interpreted under the guidance of a doctor.
How is Iron Deficiency Anaemia Treated?

The treatment of iron deficiency anaemia involves replenishing the iron stores in the body as well as identifying and treating the underlying cause if necessary.
Iron is usually provided in the form of a tablet or occasionally intravenously (IV). Iron may also be given in liquid form for infants and children. The following approaches can help maximise the absorption of iron:
- Take your iron supplements on an empty stomach. But if it causes stomach aches, you can take it with your meal.
- Take iron in combination with Vitamin C or Vitamin C-containing food/drinks, as it increases iron absorption.
- Do not take iron at the same time as antacid medications, as they decrease iron absorption. If you require antacids, make sure to take them two hours before or four hours after you take the antacid.
Additionally, eating iron-rich foods such as meat, eggs, and leafy green vegetables (e.g., kale and spinach) can help boost your body’s iron stores. For children who may be picky eaters, there are special iron-fortified cereals available as well.
Depending on the underlying cause of iron deficiency anaemia, management may range from medications to reduce heavy menses to the treatment of any sites of bleeding or ulceration in the gastrointestinal tract, etc.
How Long Does it Take for the Iron Supplements to Work?
Although oral supplements typically start to work in about three to seven days, it generally takes around two to three weeks for the symptoms of iron deficiency anaemia to improve. Your iron stores will usually be replenished after three months of iron supplementation. Supplementation may also be continued for a few months to ensure iron deficiency anaemia does not recur.
Constipation and greyish-black stools are the most common side effects associated with iron supplementation, but constipation can be managed with laxatives. Overall, the benefits of iron supplementation outweigh the side effects, and you should continue taking them until the doctor has confirmed that your iron stores have been replenished.
Is Iron Deficiency Anaemia Permanent?
No, not necessarily, but this will depend on the treatment of the causalfactor. In easily treatable causes like heavy menstrual bleeding or dietary shortages, treating the root cause will most likely cure the anaemia. However, in causes related to chronic blood loss from various sites in the body, the resolution of iron deficiency anaemia largely depends on how effectively the cause can be addressed.
What happens if Iron Deficiency Anaemia is not treated?
If left untreated, iron deficiency anaemia can have a significant impact on your health. A low blood count can put you at increased risk of heart attacks, tachycardia (rapid heart rate of more than 100 beats per minute) and a decrease in your ability to exercise normally. Additionally, low iron decreases your immunity and increases your risk of getting infections.
In pregnancy, severe iron deficiency anaemia increases the risk of a premature baby (born before 36 weeks). It is also associated with postpartum depression in the mother.
Summary

In conclusion, iron deficiency anaemia is a very common cause of anaemia and may have an immense impact on your health if left untreated. Fortunately, it is treatable with a combination of supplements and management of the underlying cause(s).
Visit Alpha Digestive & Liver Centre
If you have any of the iron deficiency symptoms mentioned above or feel you may be in the high-risk group, do reach out to our team at Alpha Digestive & Liver Centre to schedule an appointment with one of Singapore’s most trusted Consultant Gastroenterologists, Dr Benjamin Yip. Not only is Dr Yip skilled in Gastroenterology, but he is also a Hepatologist. He can provide effective medical guidance on anaemia management, especially with regards to advanced liver disease which can be a potential cause of anaemia.
References
- https://www.mayoclinic.org/diseases-conditions/anemia/symptoms-causes
- https://www.healthline.com/health/iron-deficiency-anemia
- https://www.hematology.org/education/patients/anemia/iron-deficiency
- https://www.nhlbi.nih.gov/health/anemia/iron-deficiency-anemia
- https://www.nhs.uk/conditions/iron-deficiency-anaemia/
- https://www.hematology.org/education/patients/anemia/iron-deficiency
- https://my.clevelandclinic.org/health/diseases/22824-iron-deficiency-anemia

