What is an Anal Fissure?
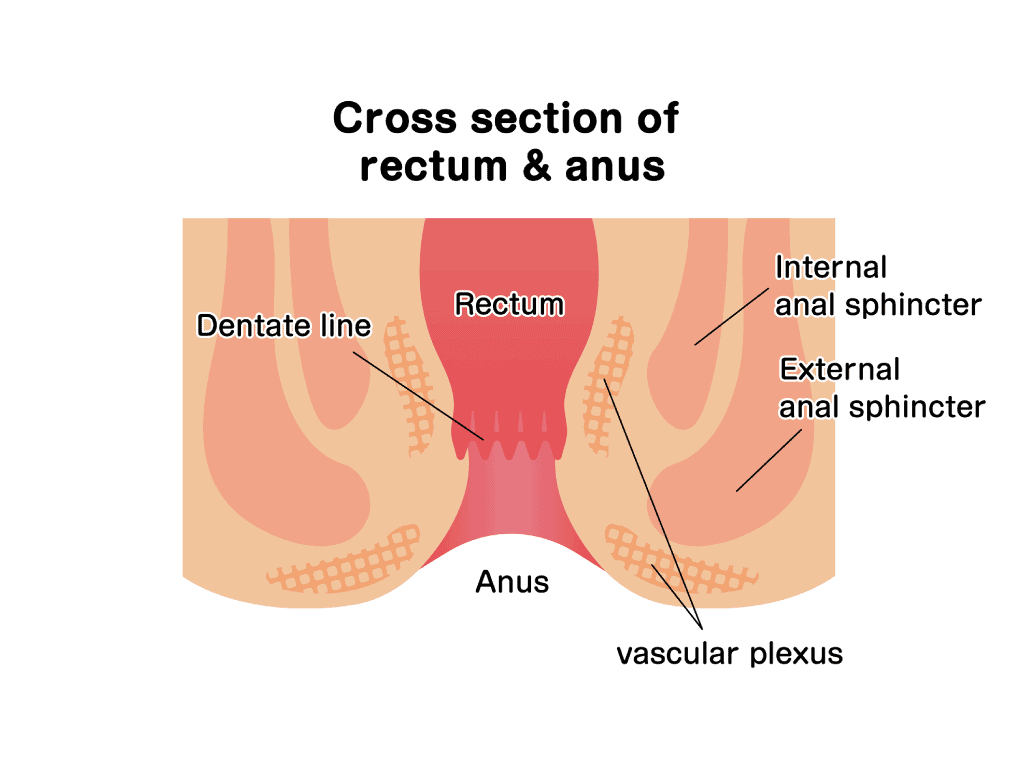
Anal fissures are a painful, but rarely serious condition that happens when there is a cut or tear in the skin surrounding your anus. It is uniquely painful as the tear exposes the anal sphincter, which is the muscle around your anus. The injury causes the sphincter to spasm and enlarge the fissure, causing further pain and discomfort.
Anal fissures generally heal after making lifestyle modifications or taking some medications. However, in severe cases, surgery may be required.
Dr Benjamin Yip cautions: “whilst anal fissures are benign and can cause rectal bleeding, colorectal cancer or other more sinister colorectal conditions can cause rectal bleeding as well.” If in doubt, do seek advice from your Gastroenterologist and consider a colonoscopy.
Common Symptoms of Anal Fissures in Singapore
Classically, patients describe anal fissures as a ‘paper cut on their anus’, with a searing or tearing pain when passing motion. The most common symptoms include:
- Pain during or after bowel movement
- Blood-coated stools or blood when wiping
- A visible tear in the skin around the anus
- Burning, painful and itching sensation around the anus
- Constipation
How is an Anal Fissure diagnosed?
An anal fissure is diagnosed by examining the skin around the anus and performing a proctoscopy. It involves the insertion of a clear, lubricated instrument into the anus to allow your doctor to visualise the anus and rectum. Further tests are rarely required to reach this diagnosis.
Anal fissures can be acute or chronic — acute fissures are those present for under 6 weeks, while chronic fissures persist beyond 6 weeks or recur frequently. Both types of fissures have unique appearances.
What does an Anal Fissure look like?
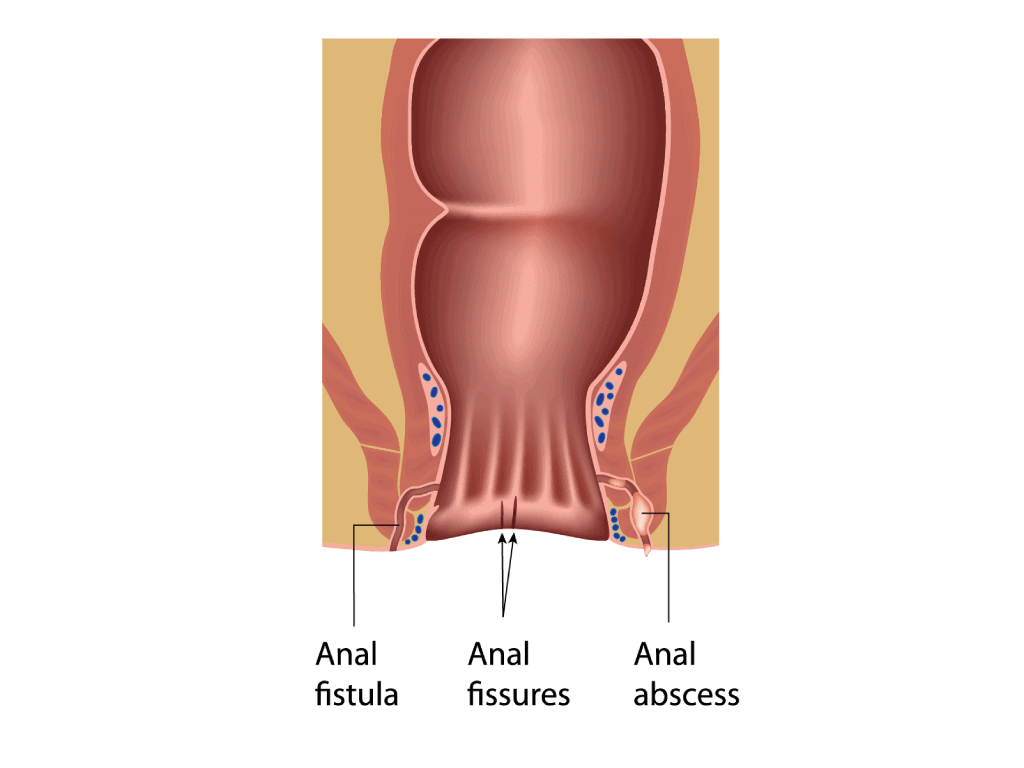
An acute anal fissure has the appearance of a paper cut and may have some redness and blood when examined. On the other hand, a chronic anal fissure usually has deeper tears, and old scarring and may have internal or external fleshy growths known as skin tags.
Anal Fissure vs Haemorrhoids
One of the main differences between the two is that anal fissures generally show symptoms during bowel movements, while haemorrhoids are painful throughout the day. Additionally, anal fissures generally resolve on their own, while haemorrhoids may require treatment.
What causes an Anal Fissure?
Anal fissures are thought to be caused by trauma to the anus or anal canal, including but not limited to:
- Chronic constipation or diarrhoea
- Excessive straining during bowel movement
- Large, hard or dry stools
- Insertion of objects into the anus
Some conditions are associated with a higher prevalence of anal fissures, such as:
- Anal cancer
- Leukaemia
- Sexually-transmitted diseases and HIV
- Inflammatory bowel diseases (IBD)
Can Anal Fissures heal on their own?
Anal fissures are similar to cuts and skin tears on other body parts and can heal fairly easily. Most anal fissures are acute, meaning they heal in under 6 weeks, usually with home treatment and basic medications such as laxatives and painkillers.
However, if left untreated and allowed to worsen over time, some complications may arise. These include:
- Constipation – Due to the pain caused by the unhealed anal fissure, one may be unable to defecate normally.
- Chronic anal fissures – a prolonged healing process can result in extensive scar tissue around the anus, forming a sentinel pile, which has the appearance of a large and usually painless skin tag.
- Anal stenosis – the anal canal may become narrowed from the formation of scar tissue around the anus or spasms of the anal sphincter.
What are the treatments available for Anal Fissures?
The majority of patients with anal fissures heal with non-surgical treatments, including a high-fibre diet, sitz baths, and medications.
Anal fissures are easily treated at home, and recurrence can also be prevented with simple lifestyle changes.
- Preventing constipation — a high-fibre diet, adequate hydration, and consumption of stool softeners or laxatives can help improve bowel movement.
- Sitz baths — soaking in a warm mixture of baking soda, salt and water for 10-20 minutes several times a day helps soothe the pain from the anal fissure and relax the anal muscles.
- Gentle wiping — after toileting, gentle wiping with cloth wipes or softer toilet paper will reduce the trauma to the anorectal area.
- Avoiding straining or prolonged sitting on the toilet.
- Applying lubrication to the anorectal area.
The above measures heal most fissures within several weeks. However, if these methods fail, or if you get anal fissures frequently, other stronger medications or interventions may be required:
- Anti-inflammatory creams — steroid-containing suppositories or creams can be applied to the anus to reduce inflammation.
- Topical relief — Various topical medications can be applied to the peri-anal region, including medication to heal the fissure or improve blood flow to the region, muscle relaxants (to relax the anal sphincter), or painkillers (if pain interferes with bowel movements).
- Botulinum toxin injections into the anal sphincter — Neurotoxin injections temporarily paralyse the anal sphincter, relieving pain and promoting healing.
When is surgery necessary for my Anal Fissure?
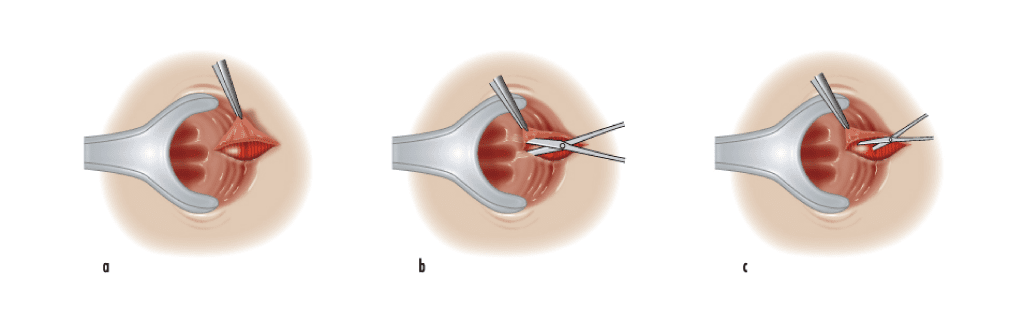
Sometimes, the fissure may not heal due to muscle spasms in the anal fissure, causing the fissure to be torn apart repeatedly and be unable to heal. If the anal fissures remain refractory to the above treatment methods, surgery may be offered in the form of lateral sphincterotomy.
This surgery entails making a small incision in the internal anal sphincter to reduce pain and spasms, allowing the wound to heal. Since the incision made is small, it does not affect one’s long-term ability to control bowel movements. This is usually done as a day surgery, meaning you can go home on the same day, a few hours after the procedure. The anal fissure should heal within a few weeks, and your doctor will review the progress subsequently.
How can I prevent Anal Fissures?
Prevention is better than cure, and there are plenty of ways to reduce the chances of getting an anal fissure:
- A high-fibre diet
- Stool softeners or laxatives if you are prone to constipation
- Good hydration and drinking plenty of water/fluids
- Avoiding excessive coffee and alcohol (as they cause dehydration)
- Regular exercise (promotes bowel movement)
- Don’t hold your urge for a bowel movement
- Avoid straining when passing motion
- Do not sit on the toilet for too long
- Keep the anal area clean and dry
- Wipe gently with cloth wipes or soft toilet paper
Summary
Anal fissures can be uncomfortable and painful, but they typically can be treated easily with simple lifestyle modifications and medications. If you suspect you have an anal fissure, do consult your gastroenterologist and seek advice on how to treat the existing injury, as well as prevent recurrence in the future.
References
- “Anal Fissure - PMC.” NCBI, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4755763/. Accessed 15 November 2022.
- “Clinical Practice Guideline for the Management of Anal Fissures.” American Society of Colon and Rectal Surgeons (ASCRS), https://fascrs.org/ascrs/media/files/downloads/Clinical%20Practice%20Guidelines/cpg_for_the_management_of_anal_fissures_jan_2017_dcr_issue.pdf. Accessed 15 November 2022.
- Villani, RD. “The management of patients with primary chronic anal fissure: a position paper.” PubMed, https://pubmed.ncbi.nlm.nih.gov/21538013/. Accessed 15 November 2022.

