What are Autoimmune Liver Diseases?
Autoimmune liver diseases occur when the body’s immune system attacks the liver and its cells, resulting in inflammation and damage. This long-term damage to the liver may cause liver scarring and fibrosis, also known as liver cirrhosis, which can eventually lead to increased risks of liver cancer and liver failure.
There are several types of autoimmune liver diseases. Common autoimmune liver diseases seen in clinical practice include autoimmune hepatitis (AIH), primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC).
Autoimmune hepatitis (AIH)
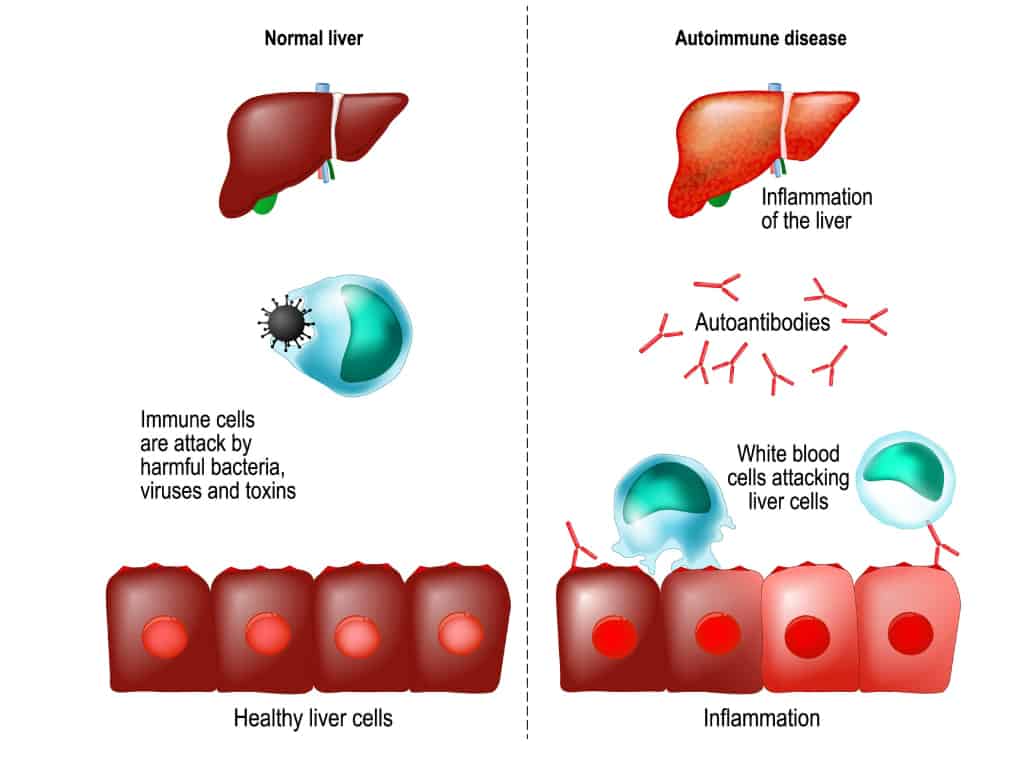
Hepatitis refers to inflammation of the liver. Autoimmune hepatitis (AIH), in turn, refers to when the body’s immune system attacks liver cells, resulting in inflammation of the liver. Advanced AIH often leads to liver cirrhosis and liver failure.
Most patients with AIH have no symptoms, and AIH is often first detected on blood tests that reveal an abnormal liver function. In severe cases, nonspecific symptoms such as:
- Fatigue
- Joint pain
- Fever
- Jaundice (yellowing of the skin and eyes, pale stools, and dark urine)
- Signs of liver impairment (generalised itching, rashes, abdominal bloating, leg swelling, abnormal blood vessels in the skin, and nausea and vomiting)
Primary Biliary Cholangitis (PBC)
Primary biliary cholangitis (PBC) is a chronic disease that can cause the gradual destruction of the bile ducts within the liver via an autoimmune process. The bile ducts connect the liver to the gut, allowing the passage of bile into the digestive tract. Bile plays a key role in food digestion as it breaks down the fat in the food we eat.
Because PBC results in bile duct damage, eventually, bile can no longer flow through the bile ducts. This then leads to the build-up of bile in the liver, causing damage to the liver cells and prolonged inflammation and scarring, which are precursors to liver cirrhosis and liver failure.
Symptoms of PBC include lethargy, itching, abdominal pain, especially over the upper right abdomen, indigestion, joint pain, diarrhoea, signs of jaundice and dry eyes and mouth. However, some patients with PBC do not experience any symptoms, in which PBC may be detected incidentally during lab tests and examinations.
Primary Sclerosing Cholangitis (PSC)
Primary Sclerosing Cholangitis (PSC) refers to chronic inflammation of the bile ducts, inside and outside the liver. This leads to scarring and, eventually, the ducts becoming narrowed or blocked, which in turn, causes liver damage. PSC is associated with inflammatory bowel disease and also puts one at greater risk of bile duct cancer (cholangiocarcinoma).
Similarly, symptoms of PSC include signs of jaundice, itching, abdominal pain, fatigue, night sweats, chills, fever, and an enlarged liver and spleen. While PBC is commonly diagnosed with blood tests and a liver biopsy, PSC is most commonly diagnosed by MRI.
Are Autoimmune Liver Diseases common?
Autoimmune liver diseases are rare overall. Autoimmune hepatitis (AIH), for instance, is a rare disease that occurs globally with a prevalence of about 10-50 cases per 100,000 people in the West. It is of an unknown cause and affects females 4 times as often as males.
Is Autoimmune Liver Disease a serious disease?
Autoimmune liver diseases, on the whole, are fairly serious conditions that should be treated promptly upon diagnosis. This is because such diseases often have the propensity to result in liver cirrhosis and liver failure if left untreated for prolonged periods of time.
What’s the difference between PBC and PSC?
PBC mainly affects the bile ducts within the liver (intrahepatic), while PSC can affect the bile ducts both inside and outside the liver. Both autoimmune liver diseases can evolve into secondary biliary cirrhosis and liver damage.
Am I at risk of developing Autoimmune Liver Diseases?
The cause of autoimmune liver diseases is largely unknown, and it is difficult to predict risk in the general population. However, if you are suffering from other autoimmune diseases such as inflammatory bowel disease, or if you have a family history of autoimmune liver diseases, it might be prudent to bring this up to your doctor and to watch out for any of the symptoms mentioned above, although it is not very possible to predict the onset and development of autoimmune liver disease as it is not clear why they develop.
How are Autoimmune Liver Diseases diagnosed?
The first step in diagnosing autoimmune liver diseases is via a blood test. This is because patients often do not experience any symptoms until the disease has progressed to cirrhosis or liver failure.
A scan (ultrasound, CT or MRI) may also be performed to examine the liver for any structural abnormalities, as well as a liver biopsy.
Dr Benjamin Yip advises that although autoimmune liver diseases are rarer, one can experience symptoms and signs attributable to more common liver diseases like fatty liver and viral hepatitis. It is wise to see your Gastroenterologist, who will perform tests to differentiate between them and achieve a definitive diagnosis, so you get prompt medical attention.
Treatment for Autoimmune Liver Diseases
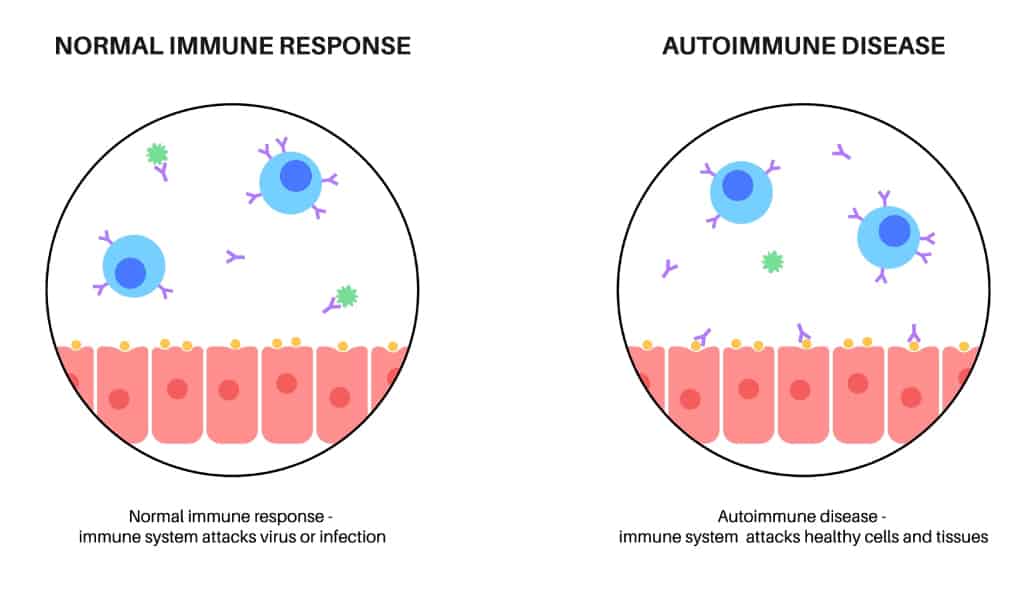
Treatment is based on which specific disease you have and how severe your symptoms are, and the patient’s current liver function. There is no cure. However, they can be controlled with medication such as steroids and other agents that help suppress the immune system. This is done to prevent further damage to the liver.
- Autoimmune hepatitis treatment involves suppressing the overactive immune system.
- Primary biliary cholangitis treatment involves improving bile flow.
- Primary sclerosing cholangitis treatment involves improving bile flow. In severe cases, a liver transplant may be recommended.
With early diagnosis and treatment, autoimmune liver diseases can be managed fairly well in current day-to-day medical care. In its early stages, proper medication may allow the liver to heal and make healthy cells again, easing the patient’s symptoms and allowing the liver to work normally.
Can Autoimmune Liver Diseases come on suddenly?
There is no fixed time of onset for autoimmune liver diseases on the whole, and the age of onset can vary greatly. Some diseases may present in both childhood and adulthood, depending on the variation, while some diseases, such as PBC, have an onset between 45-65 years old.
Can Stress cause Autoimmune Liver Diseases?
There is no association between stress and the development of autoimmune liver disease in the current literature. However, certain studies have shown that for Type 1 AIH, stress is significantly associated with relapse rates, so management of AIH may benefit from strategies that promote enhanced psychological well-being.
How long can you live with Autoimmune Liver Disease?
The prognosis of autoimmune liver disease depends on the type of disease and certain factors, such as liver function on diagnosis.
In terms of AIH, most patients who respond to treatment have a good prognosis, with the majority achieving remission and 10-year survival rates being up to 83.8 to 94%. Most patients need lifelong maintenance therapy in view of the high relapse rates of AIH. In those with liver cirrhosis on diagnosis, 10-year life expectancy was 64%.
In patients with PBC, the prognosis is highly variable and depends on different predictors such as the age of diagnosis, liver function, and clinical symptoms. If left untreated, or diagnosed late, PBC usually progresses to terminal stages over 15 to 20 years, although this is highly variable. Once symptoms develop, the median life expectancy is about 10 years.
However, quality of life is not diminished for many years in those with PBC, and patients who do not have symptoms at the time of diagnosis may continue to remain symptom-free for years. Liver transplants in terminal diseases may help improve survival outcomes.
Summary
Autoimmune liver diseases refer to conditions that lead to the destruction of liver cells by the body’s own immune system. While rare, autoimmune liver diseases can lead to severe outcomes if left untreated and undiagnosed for a long time.
If you experience any symptoms mentioned above, please visit your Gastroenterologist for a proper diagnosis and treatment plan tailored to your needs and lifestyle.
References
- “Autoimmune Hepatitis.” Cleveland Clinic, https://my.clevelandclinic.org/departments/digestive/medical-professionals/hepatology/autoimmune-hepatitis. Accessed 14 December 2022.
- “Eating, Diet, & Nutrition for Autoimmune Hepatitis | NIDDK.” National Institute of Diabetes and Digestive and Kidney Diseases, https://www.niddk.nih.gov/health-information/liver-disease/autoimmune-hepatitis/eating-diet-nutrition. Accessed 14 December 2022.
- Heneghan, Michael A. “Patient education: Autoimmune hepatitis (Beyond the Basics).” Uptodate, 14 January 2022, https://www.uptodate.com/contents/autoimmune-hepatitis-beyond-the-basics#H7. Accessed 14 December 2022.
- Lee, Tae Hoon, and James J. Peters. “Primary Biliary Cholangitis (PBC) - Hepatic and Biliary Disorders - MSD Manual Professional Edition.” MSD Manuals, https://www.msdmanuals.com/en-sg/professional/hepatic-and-biliary-disorders/fibrosis-and-cirrhosis/primary-biliary-cholangitis-pbc. Accessed 14 December 2022.
- “LiverTox: Clinical and Research Information on Drug-Induced Liver Injury.” National Library of Medicine, National Center of Biotechnology Information, 11 July 2020, https://www.ncbi.nlm.nih.gov/books/NBK548188. Accessed 14 December 2022.
- Manns, Michael P. “Autoimmune Hepatitis: The Dilemma of Rare Diseases.” Gastroenterology Journal, ScienceDirect, 26 April 2011, https://www.gastrojournal.org/article/S0016-5085(11)00537-3/fulltext. Accessed 14 December 2022.
- “Primary Biliary Cholangitis - NORD.” National Organization for Rare Disorders, https://rarediseases.org/rare-diseases/primary-biliary-cholangitis. Accessed 14 December 2022.
- Srivastava, Savita, and James L. Boyer. “Psychological stress is associated with relapse in type 1 autoimmune hepatitis.” NCBI, 16 September 2010, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3735904/. Accessed 14 December 2022.

