What is Fatty Liver?
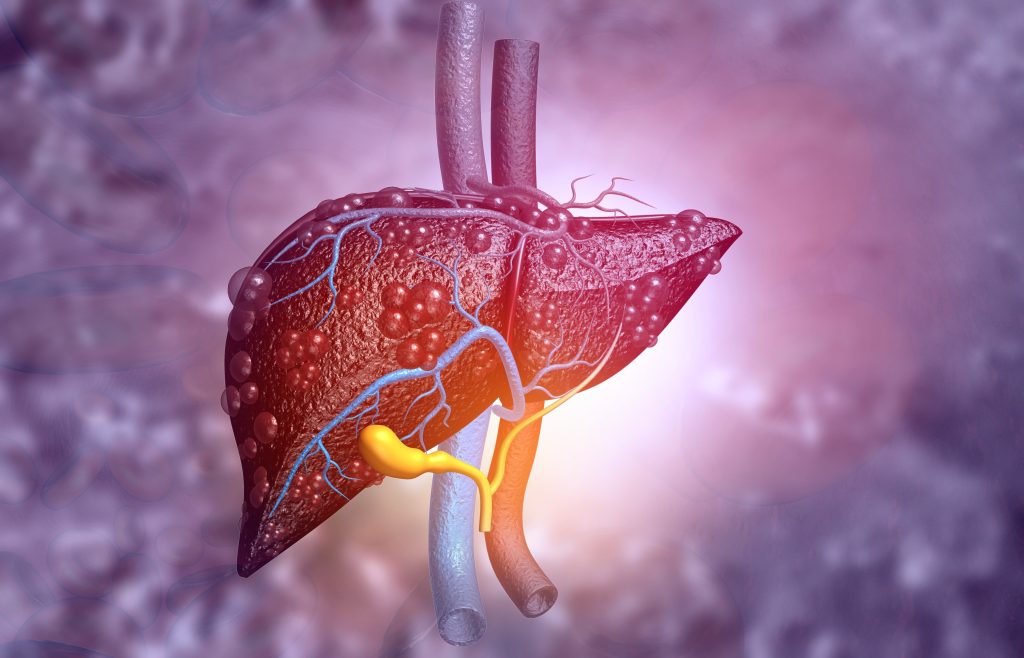
Fatty liver disease, also known as hepatic steatosis, is a common condition in Singapore. A study by SingHealth doctors claims that the incidence of the disease is rising rapidly, possibly affecting half of the population of adults in the country. The condition occurs when there is a build-up of fat in the liver, thereby making the liver susceptible to inflammation and scarring, resulting in a poorly functioning liver. It is imperative to consult a liver doctor in Singapore to treat the disease.
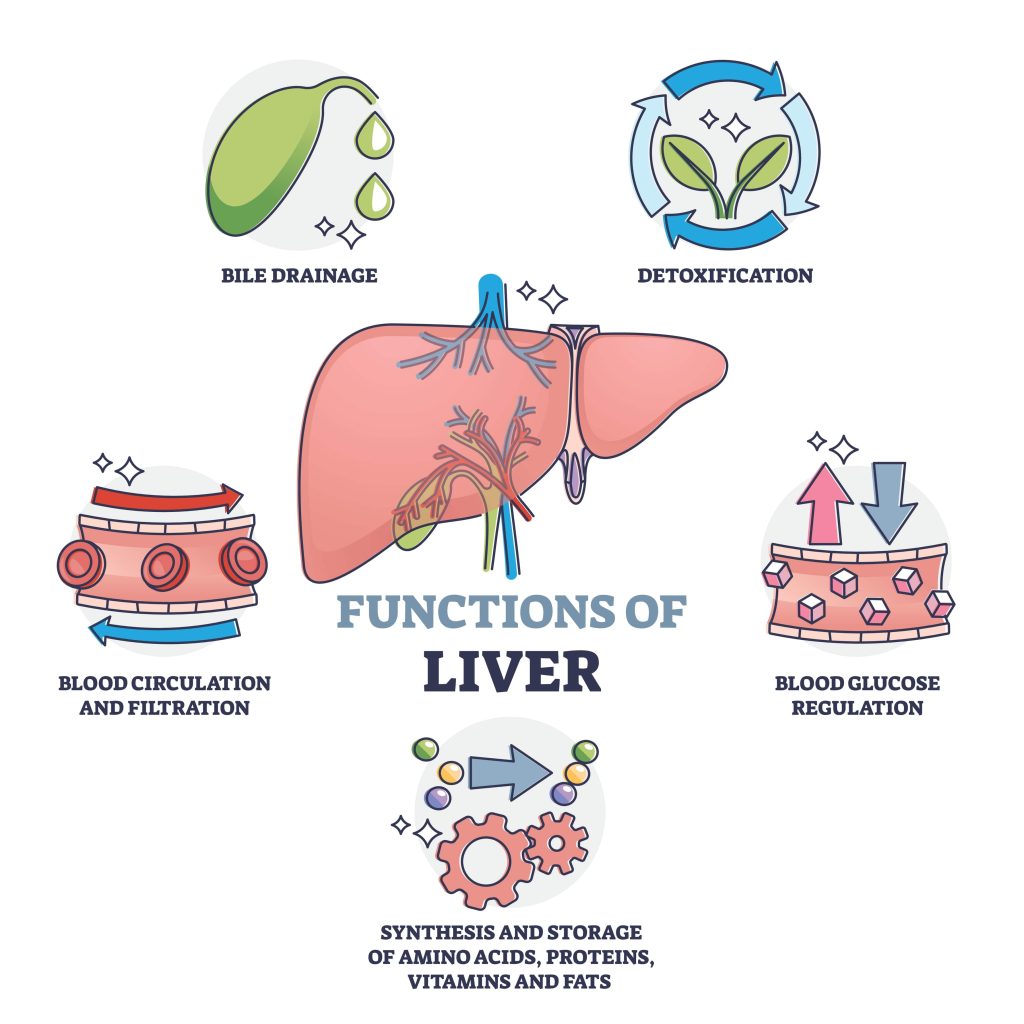
What does the Liver Do?
The liver plays an essential role in the digestive system. Its main functions are detoxification, protein synthesis, and digestion. The liver also helps with metabolism, blood filtration, and storing nutrients.
What Happens When You Have Fatty Liver Disease?
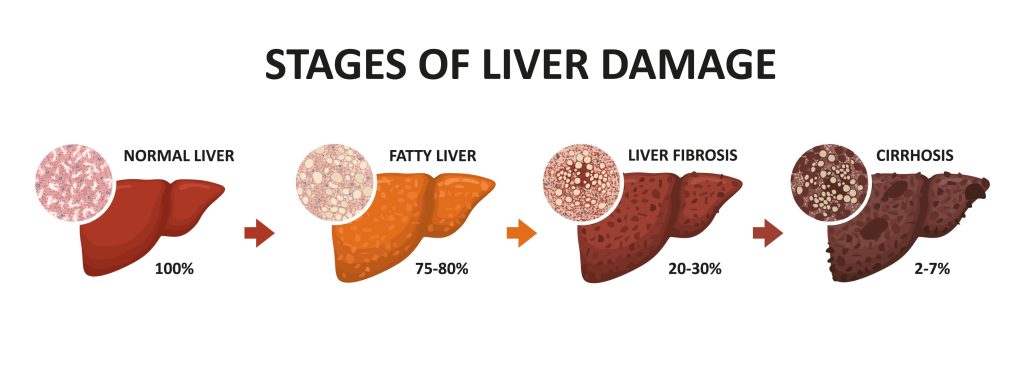
A fatty liver often presents with no symptoms until the condition progresses to hepatitis (liver inflammation) or cirrhosis (scarring) of the liver. In more severe cases, this can lead to liver failure — both of which are life-threatening conditions.
If you suspect that you suffer from this disease, we recommend that you contact us at Alpha Digestive and Liver Centre to consult an experienced liver doctor in Singapore for personalised treatment solutions.
What Are the Types of Fatty Liver disease?
Non-Alcoholic Fatty Liver Disease (NAFLD)
Non-Alcoholic Fatty Liver Disease affects people who drink little to no alcohol. NAFLD is becoming increasingly common due to the rise in obesity and diabetes, and is the most common cause of liver disease.
Two types of NAFLD are possible:
- Simple Fatty Liver, where fat is present in the liver but no inflammation or damage to the liver has occurred.
- Nonalcoholic steatohepatitis (NASH), where inflammation and liver cell damage have occurred. This might lead to extensive scarring of the liver, also termed as cirrhosis, or liver cancer.
Alcoholic Fatty Liver Disease (AFLD)
Alcoholic Fatty Liver Disease affects heavy alcohol users. As the liver breaks down the alcohol consumed, harmful substances are produced, which can cause inflammation and damage to the liver.
Acute Fatty Liver of Pregnancy (AFLP)
Acute Fatty Liver of Pregnancy is a metabolic disorder that occurs during the third trimester of pregnancy. AFLP is potentially fatal and is treated by delivering the baby as soon as possible. Usually, AFLP goes away after the baby is delivered and does not recur.
Would the Type of Alcohol I Consume Affect My Risk of Fatty Liver Disease?
Contrary to popular belief, the type of alcohol does not make a difference. It is more important to take note of how much you drink. Studies suggest that fatty liver disease affects 9 out of 10 people who drink more than 40g of alcohol a day.
What Causes Fatty Liver Disease?
Certain risk factors can predispose someone to develop fatty liver disease. However, the main cause would be eating calories in excess, as this leads to fat build-up in the liver.
Who is at Risk of Developing Fatty Liver?
Fatty liver disease is more common in those with:
- Type 2 diabetes
- Obesity (BMI above 30)
- High blood pressure
- High cholesterol and triglycerides levels
- Hormonal disorders
- Heavy drinkers
What are the Symptoms of Fatty Liver?
Most people with fatty liver disease generally have no symptoms, but some might experience abdominal pain around the area of the liver, fatigue and nausea.
As the liver condition deteriorates, other fatty liver symptoms may surface, such as:
- Fluid buildup in the abdomen and legs
- Yellowing skin and eyes
- Being prone to bruises and abnormal bleeding
- Mental confusion
- Lighter - coloured stools
- Nausea
- Weakness and fatigue
- Weight loss
- Abdominal pain
How is Fatty Liver Diagnosed?
To diagnose fatty liver disease, your gastroenterologist may recommend some of the following:
- Blood tests – High levels of liver enzymes, such as alanine aminotransferase (ALT) or aspartate aminotransferase (AST), detected in the blood is a sign of a fatty liver. Blood tests can also be used to exclude other liver conditions like viral hepatitis.
- Imaging tests – Ultrasound or computed tomography (CT scan) to visualise liver abnormalities.
- FibroScan® – A specialised ultrasound that looks for the amount of fat and scarring of the liver.
- Liver biopsy – A tissue sample is taken and examined under a microscope to determine the progression of liver disease. As this procedure is more invasive than other tests, it is usually used when the liver disease is advanced.
Prior to these tests, your doctor will also conduct a physical exam and ask you about your personal and family medical history in detail. Do inform your doctor if you have been experiencing fatigue or loss of appetite.
What are The Treatments for Fatty Liver?

The nature of fatty liver treatment you undergo depends on whether you have cirrhosis.
Without Cirrhosis
Treatment for fatty liver without cirrhosis involves addressing the cause and risk factors of fatty liver. Modifying your lifestyle is the first step to treating fatty liver disease. This involves abstaining from alcohol, losing weight, exercising more and eating more nutrient-rich foods that are low in unhealthy fat.
Liver damage can be controlled or reversed in some cases. Vitamin E and thiazolidinediones could be prescribed to treat non-alcoholic fatty liver disease in the short term. As some drugs might cause NAFLD, your doctor may advise you to stop taking those medicines.
With Cirrhosis
If the cirrhosis is severe and results in liver failure, a liver transplant is required. This is the last option for conditions that have failed to be controlled by other means.
What Complications Can Arise if Fatty Liver is Left Untreated?
If left untreated, fatty liver disease could progress to hepatitis and then to fibrosis when scar tissue becomes visible, and subsequently liver cirrhosis, where the liver is permanently scarred and hardened. Liver cancer and other liver-related illnesses might also develop. Thus, it is crucial to treat fatty liver disease at its early stages for better chances of retaining or restoring liver function.
Dr Benjamin Yip highlights the importance of scheduling routine check-ups as fatty liver is rapidly becoming the most common liver disease, driven by the increasing prevalence of overweight and obesity. If you have any of the the aforementioned symptoms and suspect it could be fatty liver, we recommend you schedule a consultation with a liver doctor in Singapore. for a comprehensive assessment. This is crucial because this disease is "silent" in the early stages, and you may already have irreversible liver damage once you start having symptoms.
Summary
Fatty liver refers to an accumulation of fats in the liver. In the early stages, people might experience no symptoms or abdominal discomfort. However, in later stages, symptoms such as fluid build-up and yellowing of skin could present themselves as signs of fatty liver. To diagnose fatty liver, blood tests, imaging tests, and a liver biopsy could be conducted.
Lifestyle and diet modifications are key in treating fatty liver as alcohol consumption, obesity, and diabetes are significant risk factors for the disease. Fatty liver should be treated promptly to prevent complications like liver fibrosis and liver cirrhosis. If you or your loved ones have any symptoms of fatty liver, do not hesitate to contact us at Alpha Digestive and Liver Centre for a consultation with our experienced gastroenterologist, Dr Benjamin Yip.
References
- 1. “Alcohol-related liver disease.” Drinkaware, https://www.drinkaware.co.uk/facts/health-effects-of-alcohol/alcohol-related-diseases/alcohol-related-liver-disease. Accessed 19 May 2022.
- 2. “Fatty Liver Disease: Risk Factors, Symptoms, Types & Prevention.” Cleveland Clinic, 31 July 2020, https://my.clevelandclinic.org/health/diseases/15831-fatty-liver-disease. Accessed 19 May 2022.
- 3. Fowler, Paige. “Fatty Liver Disease: Nonalcoholic & Alcoholic Steatohepatitis (NAFLD/AFLD).” WebMD, 4 November 2021, 4 https://www.webmd.com/hepatitis/fatty-liver-disease. Accessed 19 May 2022.
- 4. Tommolino, Emily, and BS Anand. “Fatty Liver: Overview, Etiology, Epidemiology.” Medscape Reference, 12 April 2018, https://emedicine.medscape.com/article/175472-overview. Accessed 19 May 2022.

