Introduction
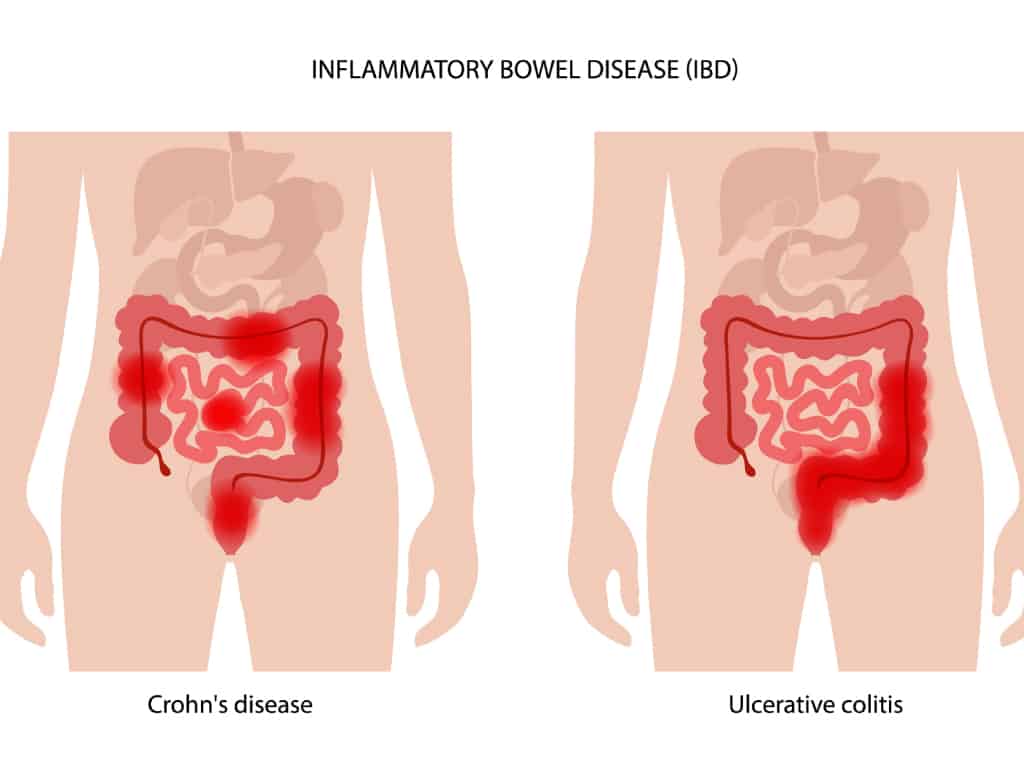
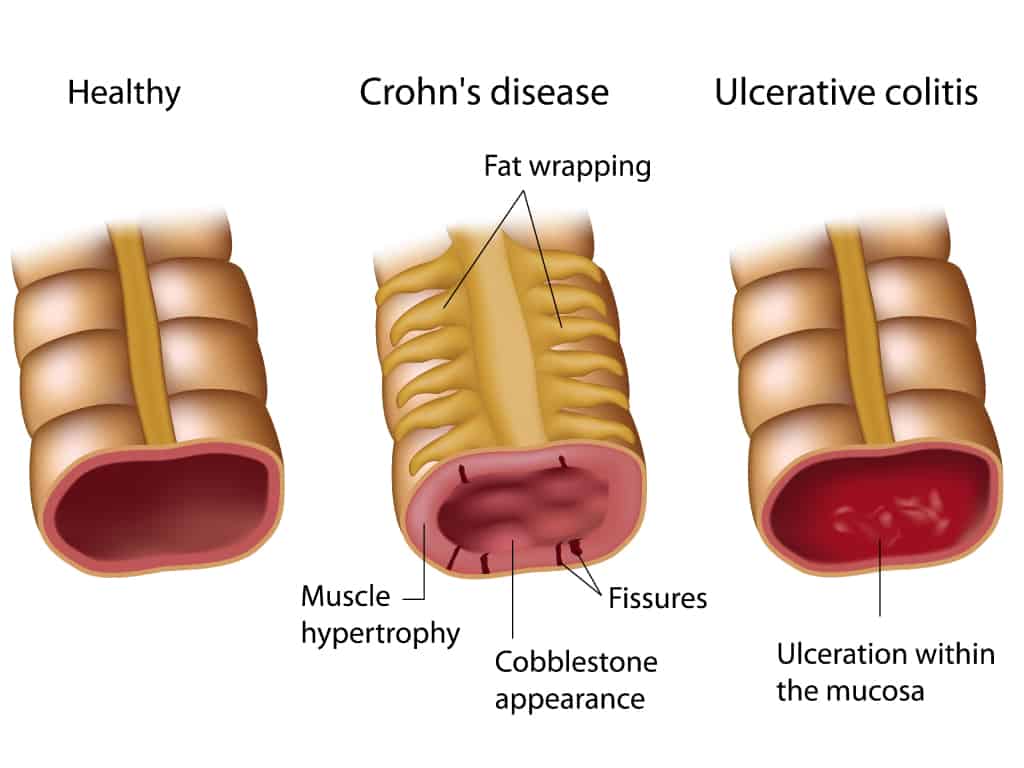
Inflammatory bowel disease (IBD) is a term describing disorders that involve chronic inflammation of tissues in the gastrointestinal (GI) tract. These include Crohn’s disease and ulcerative colitis (UC).
UC causes inflammation only in the lining of the colon and rectum, while Crohn’s disease most commonly affects the small intestine, but can occur anywhere within the GI tract. IBD can range from mild to severe and can be life-threatening in some cases.
How is IBD caused?
The exact cause of IBD remains unknown, but there are several possible causes that can contribute to it.
- IBD can be the result of an immune system malfunction wherein an atypical immune response causes the immune system to attack cells in the digestive tract while fighting off an invading virus.
- It can also be hereditary and associated with several gene mutations.
Common symptoms of Inflammatory Bowel Disease
As the name suggests, IBD is characterised by chronic inflammation of the gastrointestinal (GI) tract. Symptoms of IBD include:
- Chronic diarrhoea
- Tiredness
- Abdominal pain or cramping
- Rectal bleeding/ bloody stools
- Reduced appetite
- Weight loss
- Skin problems
- Fever
- Joint pain
IBS vs IBD - how can you tell?
IBD can be confused with IBS, but IBS is less severe and does not involve inflammation of the GI tract. IBS does not typically cause unintentional weight loss. IBS is a functional disease that does not typically show up on tests, but IBD is a structural disease that causes physical damage that can be seen.
How is IBD diagnosed?
IBD can be diagnosed through tests and procedures, which include:
Colonoscopy
A colonoscopy is a procedure in which a doctor inserts a soft and flexible tube with a built-in camera into the anus in order to examine the lining of the colon. A biopsy may be taken to diagnose IBD.
Oesophago-gastro-duodenoscopy (OGD)
This procedure is also known as gastroscopy, wherein a soft and flexible tube with a camera is inserted into the mouth in order to examine the lining of the oesophagus, stomach, and the first section of the small intestine.
CT scan
A CT scan allows doctors to look at the entire bowel as well as tissues outside the bowel to check for inflammation.
MRI scan
An MRI scan helps to visualise soft tissues like the intestinal lining, and may reveal small tears or ulcers.
How is IBD treated?
IBD cannot be cured, but treatment can help to relieve symptoms and allow for long-term remission and reduced risks of complications. IBD treatment usually comprises medication and surgery.
A high frequency of flare-ups should be avoided, and the progression of the inflammation should be prevented to prevent irreversible bowel damage.
Common medications used to treat IBD include:
Anti-inflammatory drugs
Anti-inflammatory medication can be prescribed to treat mild to moderate cases of IBD, and common drugs include mesalamine, balsalazide, and olsalazine.
Immunosuppressants
These drugs suppress the immune response that releases chemicals that induce inflammation and damage the lining of the GI tract. Some common examples include azathioprine, mercaptopurine, and methotrexate.
Biologics
These neutralise proteins in the body that cause inflammation, usually administered intravenously or through injections. Some common examples include infliximab, adalimumab and golimumab.
Surgery
For cases of IBD where symptoms are not relieved by drugs, surgery may be recommended. For UC, surgery involves the removal of the colon and rectum in their entirety, with an internal pouch attached to the anus that allows for bowel movements.
For Crohn’s disease, damaged portions of the GI tract may be removed, or surgery may be used to close fistulas and drain abscesses.
Can IBD cause stomach cancer?
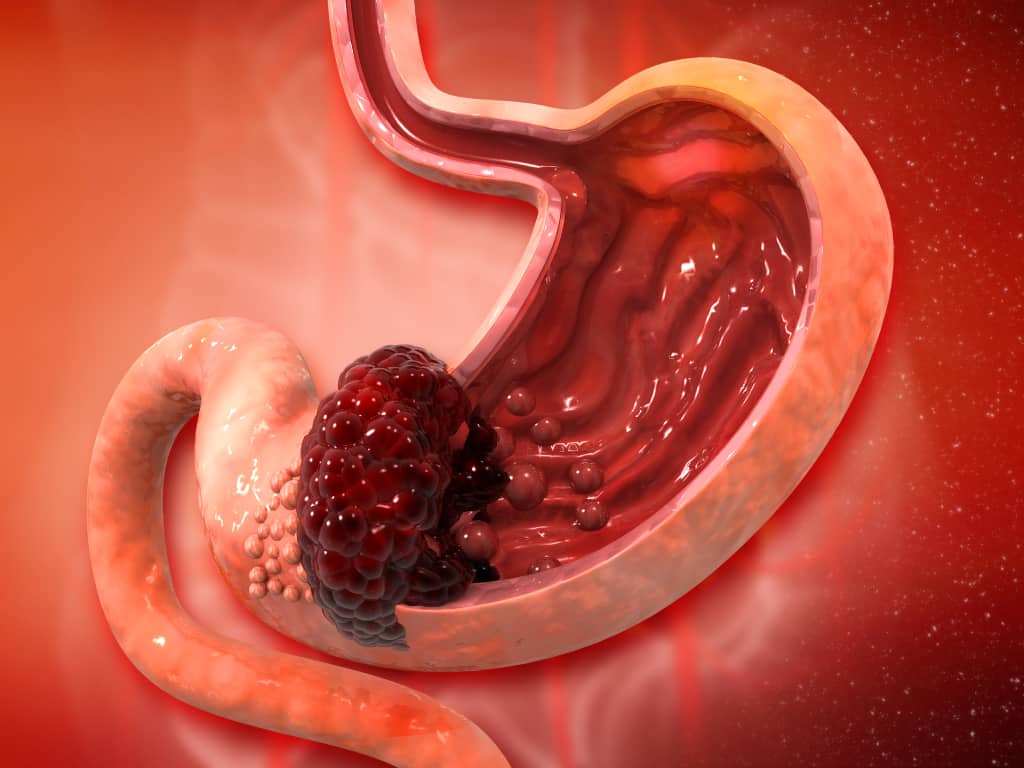
IBD is a primary risk factor for stomach cancer, especially in patients with Crohn’s disease. This is because the continuous turnover of the cells lining the intestinal walls could increase the chances of irregularities that cause cancer.
Foods to avoid with IBD
A good IBD diet helps to improve inflammation, and certain foods can trigger symptoms and, thus, should be avoided. These include:
- Fatty, greasy or fried food
- Spicy food
- Caffeinated, sugary or alcoholic beverages
- Raw, high-fibre fruits and vegetables
- Sweets and other sources of added sugar
Can IBD go away on its own?
IBD cannot be cured, and does not go into remission without treatment. If left untreated, IBD can lead to serious and possibly life-threatening complications. These include, but are not limited to, blood clots, inflammation in other areas of the body, malnutrition, fistulas, bowel obstructions or toxic megacolon.
Summary
IBD is a chronic and lifelong disease that ranges from moderate to severe but can be managed with proper treatment, diet, and lifestyle changes. Dr Benjamin Yip cautions, “IBD is becoming more common in the Asia Pacific region, including Singapore. If left untreated, these conditions can develop into severe or even life-threatening complications.” If in doubt, please consult your Gastroenterologist for a proper diagnosis and personalised treatment plan.
References
- “Inflammatory Bowel Disease.” PubMed, 27 June 2022, https://pubmed.ncbi.nlm.nih.gov/29262182/. Accessed 14 December 2022.
- “What is inflammatory bowel disease (IBD)? | IBD.” CDC, https://www.cdc.gov/ibd/what-is-IBD.htm#. Accessed 14 December 2022.
- “What to Eat & What to Avoid to Manage Your IBD.” The Iowa Clinic, 4 September 2020, https://www.iowaclinic.com/gastroenterology/ibd-food-what-eat/. Accessed 14 December 2022.

