What is Malabsorption?
Malabsorption is a common group of disorders characterised by the body’s ineffective absorption of nutrients from food in Singapore. Malabsorption can be acute or chronic, with varying symptoms depending on the type of malabsorption.
There are many different causes, ranging from enzyme deficiencies leading to the inability to absorb certain types of food (e.g. lactose intolerance), to diseases affecting the gastrointestinal tract (e.g. infections, celiac disease). Other less common causes include diseases affecting the pancreas or bile ducts, Crohn’s disease, or bowel surgery (e.g. short bowel syndrome after bowel resection surgery).
In the long run, it can lead to malnutrition of both macro and micronutrients and have an impact on your health. In this article, we will be sharing about the more common types of malabsorption and their causes, symptoms and treatment options.
What are the symptoms and types of Malabsorption?
There are two broad categories of malabsorption: general malabsorption, which means absorption of all substances are equally affected, and malabsorption of specific food types.
In general malabsorption, patients most frequently present with abdominal pain, bloating, gas or soft stools/diarrhoea. This is because the body excretes whatever cannot be absorbed by the intestines, reducing the transit time of food in your gut, passing out as brown or green stools.
For malabsorption of specific food types, we will briefly cover the causes and symptoms of fat, bile salt, carbohydrate and protein malabsorption.
Fat malabsorption
This is one of the most common types of malabsorption, and has a wide variety of causes, including (but not limited to) bile duct obstruction, celiac disease, short bowel syndrome, pancreatic diseases or gut infections.
When one eats fat-containing or oily food, fats and fat-soluble vitamins are unable to be absorbed and passed out as fatty stools, termed “steatorrhea”. The stools float on top of the water, have an oily, pale yellow appearance and are foul-smelling.
Bile salt malabsorption
Bile salts are normally secreted into the small intestine to aid with digestion, then reabsorbed later on. In bile salt malabsorption, the bile salts instead travel through the gut. The concentrated bile salts leads to additional water being retained inside the intestines, causing green-coloured diarrhoea.
Common causes of bile acid malabsorption are small intestine resection or diseases affecting the terminal ileum (eg. Crohn's disease and enteritis), resulting in a loss of bile acid transporters and hence malabsorption.
Protein malabsorption
Protein malabsorption is usually associated with specific enzyme deficiencies that lead to an inability to break down different proteins. Examples of this include gluten intolerance. Symptoms include feeling bloated, fatigued or having abdominal pain after taking gluten-containing foods like pastries, pasta, cereal, beer, etc.
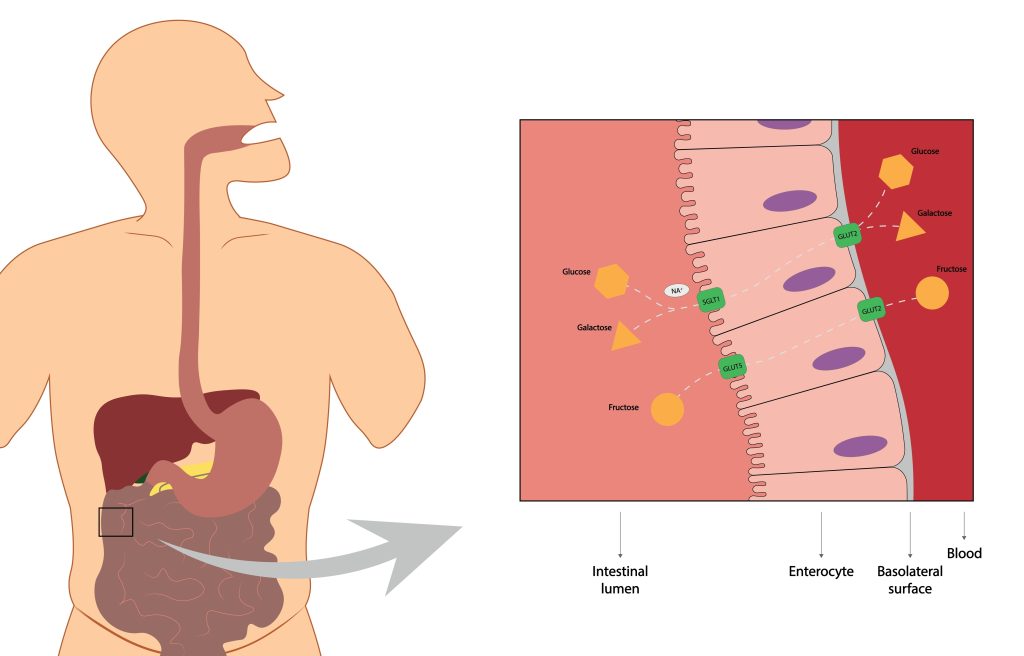
Carbohydrate malabsorption
This occurs due to defective absorption of dietary carbohydrates, sugars and starches.This includes sugar-containing foods, dessert, drinks, as well as starch/carbohydrates like potato and rice. Eating foods containing these results predominantly in bloating and gas.
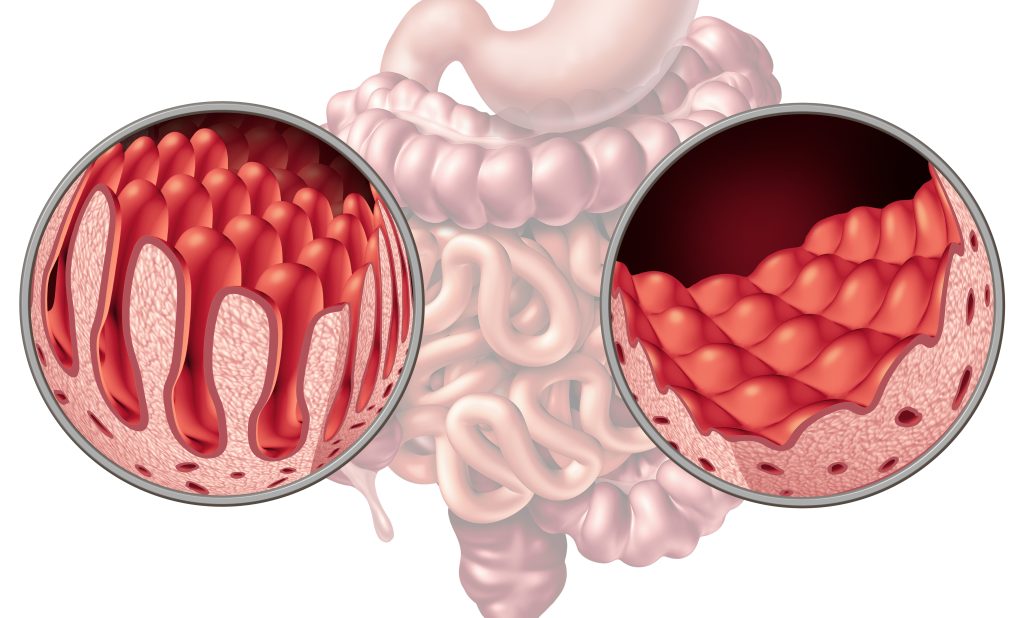
The most well-known example of carbohydrate malabsorption is lactose intolerance, a common affliction in Asian populations. It can be caused by an enzyme deficiency (lactase), resulting in cramping, distention or diarrhoea after eating foods containing dairy products. Causes also include acute gastroenteritis (stomach flu), celiac disease, and other conditions that affect the intestinal lining’s ability to produce lactase, the enzyme that breaks down lactose.
Maldigestion or Malabsorption?
Occasionally, you may come across the term maldigestion. The difference between the definition of maldigestion and malabsorption is a very technical one, but overall, the clinical presentation and complications of maldigestion and malabsorption are similar. Maldigestion is the ineffective breakdown of nutrients, while malabsorption refers to ineffective absorption of nutrients.
Whether it’s due to poor digestion or poor absorption, both conditions result in the suboptimal intake of nutrients from food into the body and have similar side effects, including nutritional deficiencies.
How is Malabsorption diagnosed?
After your consultation with a doctor, you may be suspected to have malabsorption syndrome. Some tests are done to ascertain the underlying cause, as well as assess for side effects and nutritional deficiencies related to the condition.
For instance, a hydrogen breath test is a very common test done to diagnose carbohydrate intolerances, including lactose intolerance, and small intestinal bacterial overgrowth. Normally, there is very little hydrogen in each exhalation, so if you have unusually high hydrogen levels, it may be an indicator of carbohydrate/sugars intolerance (as the faulty breakdown results in hydrogen production) or small intestine bacterial overgrowth (as bacteria generate hydrogen). Dr Benjamin Yip comments: “A hydrogen breath test may be key to finding out what type of malabsorption one suffers from so that treatment can be tailored”.
Stool tests can be used as well, to rule out infectious causes of your diarrhoea-like symptoms (e.g. bacteria, parasites), as well as test the amount of fat in your stools to diagnose fat malabsorption.
Since nutritional deficiencies are common in malabsorption, general blood tests such as a full blood count and the levels of various vitamins may be taken, to assess for any anaemia (low blood count) or vitamin deficiencies.
An endoscopy or colonoscopy may also be offered, to allow your doctor to directly visualise your oesophagus, stomach and intestines, to assess for any underlying disease, and to screen for other causes of your symptoms such as inflammatory bowel disease, cancer, etc.
How is Malabsorption treated?
In general, supplements and nutrition advice from a dietician may be useful in replacing the nutrients one is deficient in. Additionally, if the malabsorption is triggered by certain food groups (e.g. carbohydrates, fats), a dietician may be able to assist with meal-planning to ensure you still receive adequate nutrients while avoiding the triggers.
If the malabsorption is caused by certain enzyme deficiencies, there are options to replace the enzyme as well. For bile acid malabsorption, a type of medication called bile acid sequestrants may be prescribed to help prevent diarrhoea after meals.
If the malabsorption is transient and caused by an acute infection, your symptoms should go away once you recover. If it’s related to certain foods, avoiding those food groups should largely resolve the symptoms. Chronic or genetic causes of malabsorption require a treatment regime tailored to the individual and the severity of the disease, often involving both medications and lifestyle intervention.
What complications could arise if Malabsorption is not treated?
If untreated or poorly managed, malabsorption can have serious health consequences caused by deficiencies in both macro and micronutrients.
Over time, signs of chronic malnutrition may appear:
- Loss of weight, wasting of muscles
- Poor immunity
- Dry skin, hair loss
- Fatigue and irritability
- Missed periods in women
- Growth delays in children
- Paleness, giddiness, weakness
In patients with fat malabsorption, various deficiencies in fat-soluble vitamins (A, D, E, K) may manifest with these symptoms:
- Vitamin A deficiency: Night blindness
- Vitamin D deficiency: Bone or joint aches, muscle pain, fatigue, weakened bones
- Vitamin E deficiency: Muscle weakness, worsening vision
- Vitamin K deficiency: Increased bleeding tendencies (gums, nose, gastrointestinal tract), easy bruising
The symptoms of all these deficiencies may overlap, and patients with malabsorption will usually be deficient in multiple types of nutrients. All these symptoms can have a significant impact on one’s physical and mental health and quality of life.
Summary
In conclusion, malabsorption syndromes are a broad group of disorders affecting nutrient absorption by the gut and may be caused by a wide variety of diseases. It is essential to identify triggers and treat the underlying cause early, as well as manage the disease long-term and prevent chronic malnutrition or micronutrient deficiencies.
If you suspect you may have malabsorption or other gastrointestinal diseases, do arrange a consultation with a medical professional to obtain a diagnosis and treatment plan.
References
- Högenauer, Christoph, and Heinz F. Hammer. “Maldigestion and Malabsorption.” Clinical Gate, 16 May 2015, https://clinicalgate.com/maldigestion-and-malabsorption/. Accessed 4 October 2022.
- “Malabsorption (Syndrome): Symptoms, Causes & Treatment.” Cleveland Clinic, 6 April 2022, https://my.clevelandclinic.org/health/diseases/22722-malabsorption. Accessed 4 October 2022.
- Ruiz, Atenodoro R. “Carbohydrate Intolerance - Gastrointestinal Disorders - MSD Manual Professional Edition.” MSD Manuals, https://www.msdmanuals.com/en-sg/professional/gastrointestinal-disorders/malabsorption-syndromes/carbohydrate-intolerance. Accessed 4 October 2022.

