What is Stomach Cancer?
Stomach cancer, also known as gastric cancer, is the 7th most common cancer among men and the 9th among women in Singapore, contributing to over 300 cancer-related deaths annually.
Cancers are often related to DNA mutations or defects that result in abnormal and unregulated cell growth into tumours. There are several risk factors for stomach cancer, including family history and lifestyle or dietary choices. Fortunately, there has been an overall downward trend in the incidence of stomach cancer globally, attributable to increased health screening, eradication of Helicobacter pylori, as well as greater awareness about its risk factors and how to prevent stomach cancer.
What are the Stages of Stomach Cancer?
The stages of cancer indicate how far the cancer has spread in the body from where it first formed. Stomach cancer has four stages, and is based on the depth of invasion of the tumour into the lining of the stomach wall, or lymph nodes and the presence of metastases. These elements will affect the treatment options, long-term prognosis, and chances of survival.
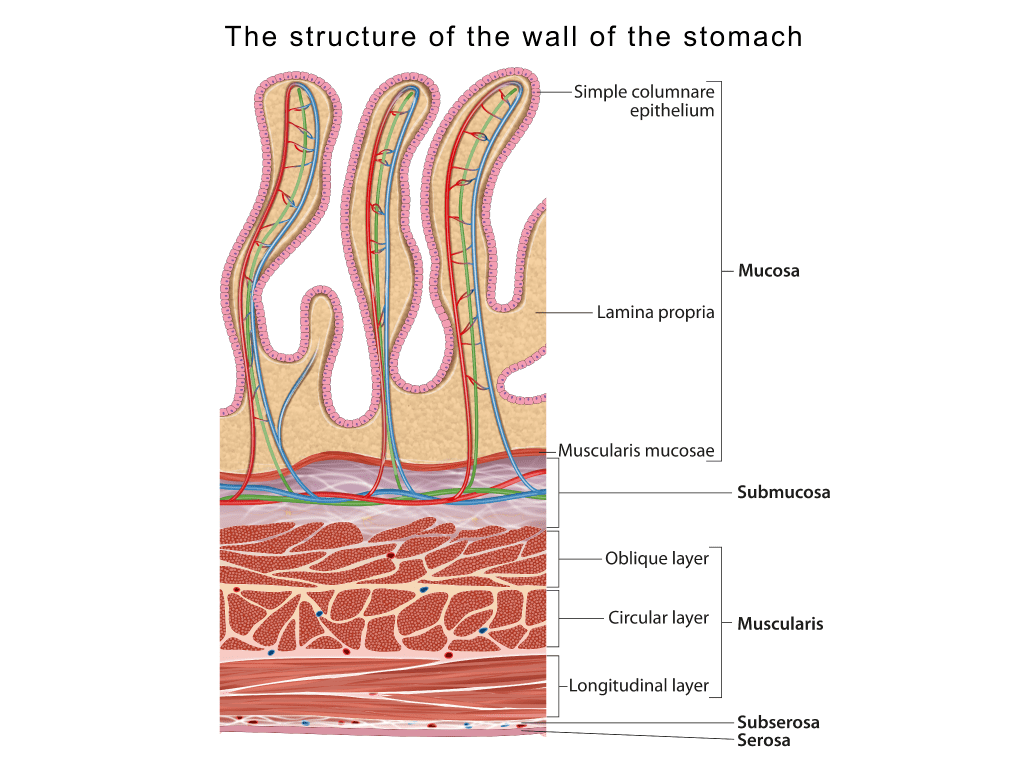
The stomach wall has five layers which will be affected by stomach cancer:
1. Mucosa: the innermost layer where most stomach cancers start growing. Stomach acid and digestive enzymes are made in this layer
2. Submucosa: a thin supporting layer
3. Muscularis propria: a muscle-containing layer that contracts the stomach during digestion
4. Subserosa: an external layer that wraps around the stomach
5. Serosa: the outermost layer
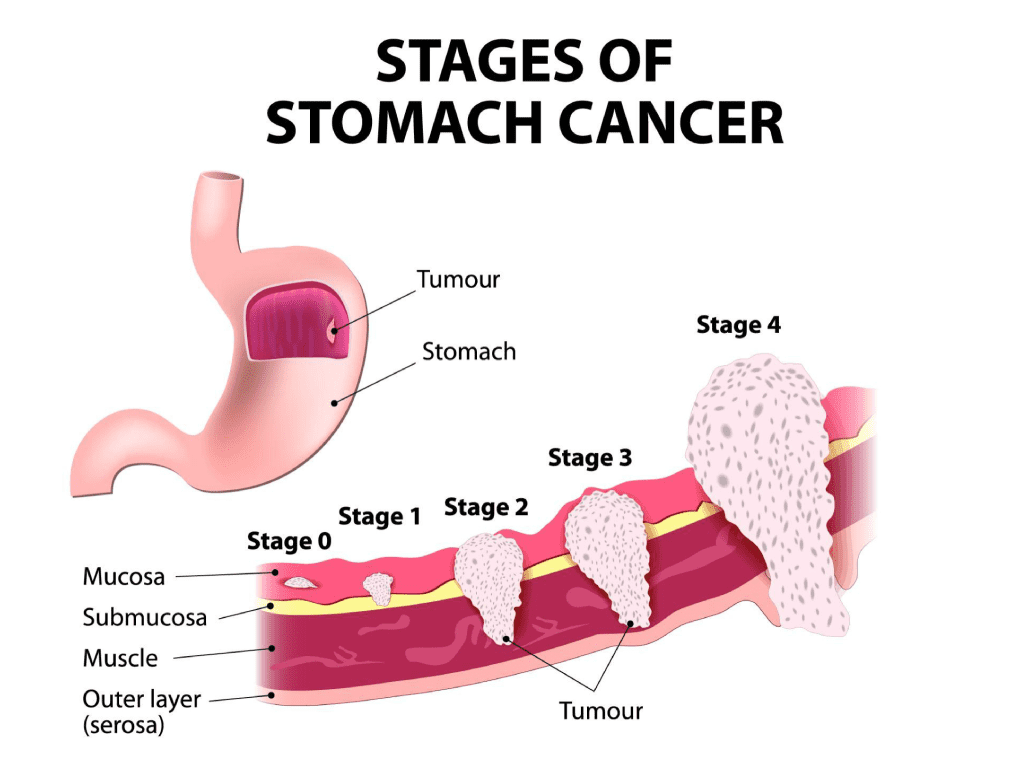
The cancer advances throughout the body, penetrating the five gastric walls as evidenced by the progression of the stomach cancer stages:
- Stage 1 (early): Tumour is within the mucosa or submucosa
- Stage 2-3 (locally advanced): Tumour has invaded the muscularis propria or subserosa, as well as nearby lymph nodes
- Stage 4 (advanced, metastatic): The tumour has spread to organs beyond the stomach or distant lymph nodes
Does Stomach Cancer Progress Quickly?
As with all cancers, there is no definite answer to how fast each case of stomach cancer will progress. It varies greatly from person to person, depending on the type and aggressiveness of the tumour, and the underlying conditions causing the cancer.
What are the Signs and Symptoms of Stomach Cancer?
There are typically no symptoms in the early stages and is usually only detected at later stages when the size of the tumour begins causing symptoms. However, there are a few signs of stomach cancer that you should be vigilant of:
- Early satiety (feeling full after eating little)
- Loss of appetite
- Bloating, especially after meals
- Difficulty swallowing, or the sensation of food being stuck
- Reflux/heartburn
- Indigestion
- Nausea, vomiting
- Tummy pain
- Unintentional weight loss
Can Stomach Cancer be Cured?
As with most cancers, if it is detected in the early stages, it is potentially curable with surgery to remove all traces of the tumour. Unfortunately, stomach cancer symptoms in the early stages are so subtle, often leading to a late diagnosis—over two-thirds of stomach cancer patients are diagnosed only at Stage 3 or 4.
For the cases that cannot be cured, it is still possible to prolong survival and manage symptoms through chemotherapy, radiotherapy or surgery.
Is Stomach Cancer Fatal?
The likelihood of survival depends on the stage and available treatment options. According to the National Cancer Institute’s data, the 5-year survival rate for localised stomach cancer (before it has spread beyond the stomach) is 70%. However, once the cancer has spread to adjacent organs or lymph nodes, the 5-year survival rate drops to 32%.
How is Stomach Cancer Diagnosed?
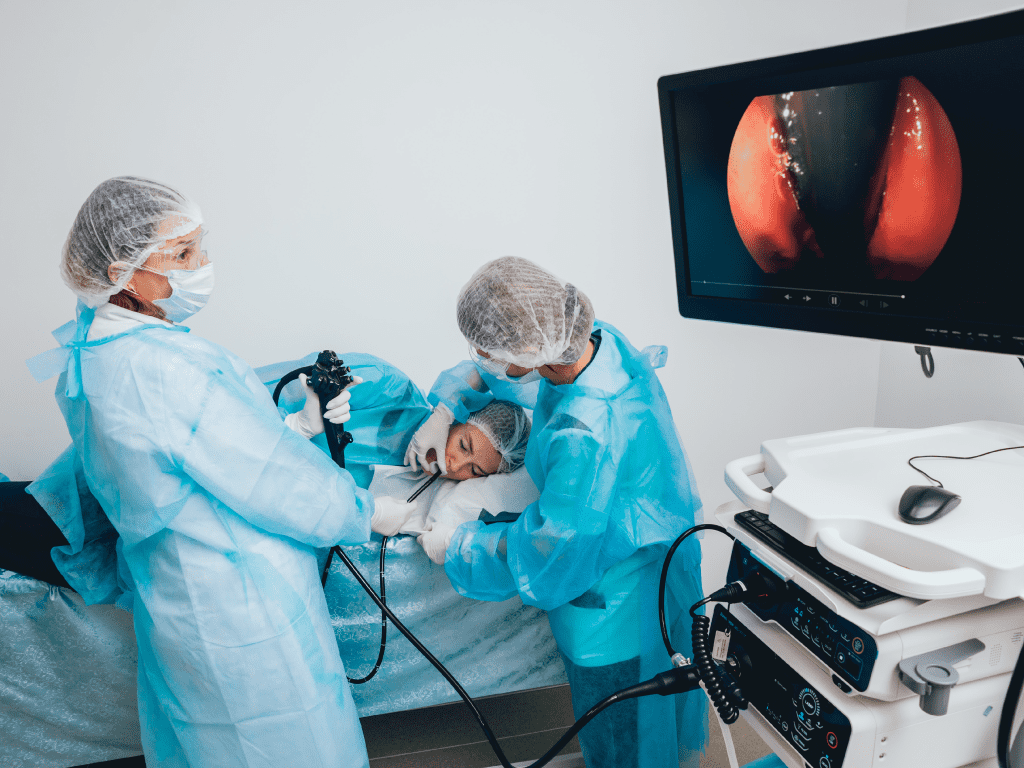
Stomach cancer is diagnosed via stomach cancer screening methods such as a gastroscopy or Oesophago-Gastro-Duodenoscopy (OGD),; they are used to visualise the oesophagus, stomach & part of the small intestine. An OGD is done by inserting a flexible, thin tube, with a camera attached to the end down your throat, enabling your doctor to visualise the structures inside your stomach and take samples of your tissue to confirm the diagnosis of cancer.
Once the diagnosis has been confirmed, the cancer has to be staged in order to determine treatment outcomes. Cancer is diagnosed based on histology (appearance of cells under the microscope), while staging is determined by the TNM system (Tumour-Nodes-Metastasis).
To determine the stage, a CT or MRI scan is done to assess the size of the tumour, depth of invasion, and whether it has spread to adjacent organs or lymph nodes. A CT scan combines multiple X-ray images into a computer system which generates cross-sectional images of your body, whereas an MRI uses strong magnets and radio waves. If there is suspicion of lymph node invasion, a lymph node biopsy may be done to obtain tissue samples for further examination under the microscope in order to determine the presence of cancer cells.
Is there a Blood test for Stomach Cancer?
Recent advancements in technology have brought about a clinically approved molecular blood test for the early detection of gastric cancer, GASTROClear.
This blood test detects cancer-related microRNA tumour marker signatures present in a patient’s blood before stomach cancer symptoms appear, with close to 90% sensitivity. This allows your gastroenterologist to assess your risk for stomach cancer and discern whether further diagnostic tests should be done.
What are the Treatments for Stomach Cancer?
There are different types of treatment for patients with gastric cancer, involving a combination of surgery, chemotherapy, radiotherapy, etc. Our cancer treatments are personalised and will be tailored by your doctor to the type, size, and stage of cancer diagnosed.
Once your gastroenterologist decides the cancer is under control, you will have regular follow-up appointments and surveillance scans or blood tests to ensure that the cancer has not recurred.
For surgery, there are various options:
- Gastrectomy: A surgery involving all (total gastrectomy) or part (subtotal gastrectomy) of the stomach being removed to eradicate the tumour.
- Endoluminal stent placement: If the tumour is blocking the opening of the stomach, a straw-like tube is inserted to maintain an opening to allow passage of food to the stomach.
- Endoluminal laser therapy: A minimally-invasive surgery that involves the insertion of an endoscope (a thin, flexible tube) down the throat. A miniature laser is attached to the end of this scope and is used to remove parts of the tumour.
- Gastrojejunostomy: A surgery that involves the removal of part of the stomach with the tumour, and reconnecting the remaining tissues to the jejunum to allow the normal passage of food.
For small, early-stage tumours, Endoscopic Mucosal Resection (EMR) or Endoscopic submucosal dissection (ESD) may be done. It is a minimally invasive procedure that helps remove tumours or precancerous growths from the lining of the stomach via an endoscope.
In combination with the above treatment, additional treatment may be given (adjuvant therapy), to lower the risk of the cancer returning. These include chemotherapy, radiation therapy, chemoradiation, targeted therapy, immunotherapy, etc.
Once your gastroenterologist believes that the cancer is under control, you will have regular follow-up appointments and surveillance scans or blood tests to ensure that the cancer has not recurred.
Who is at Risk for Stomach Cancer?
There are various well-known risk factors for stomach cancer:
- Chronic infection with Helicobacter Pylori (a bacteria that causes stomach inflammation/ulcers/cancers)
- Chronic gastritis (inflammation of the stomach lining)
- Family history of stomach cancer or other gastrointestinal cancers
- Consumption of unhealthy foods, including smoked foods, salted fish/meat, or pickled foods
- High consumption of alcohol
- Smoking
- A diet without adequate fruits and vegetables
The presence of these alone does not mean you definitely will get stomach cancer; conversely, some stomach cancer patients may have none of these risk factors.
Our gastroenterologist at Alpha Digestive Liver Centre, Dr Benjamin Yip cautions that whilst colorectal cancer screening is widely known, stomach cancer screening is relatively unknown. If you have the risk factors mentioned in this article, it is important to discuss with your Gastroenterologist how best to screen for stomach cancer.
Can Young People in their 20s-30s Get Stomach Cancer Too?
Unfortunately, stomach cancer can affect people of all ages, and the survival rate tends to be worse for younger people due to late detection.
As stomach cancer is more common in the elderly, the diagnosis of cancer in younger adults is often overlooked, even when they present with symptoms suggesting the presence of stomach cancer. By the time the cancer is detected, the cancer may have reached a more advanced stage. This, in turn, delays treatment and results in an average survival of less than 6 months.
If you are a young person with a family history of cancer, especially gastrointestinal cancers, it is important to go for regular screening and be vigilant for any stomach cancer symptoms.
How Can I Prevent Myself from Getting Stomach Cancer (Again)?
Adopting healthy dietary and lifestyle measures, as well as routine cancer screening, are the easiest ways you can reduce your risk of stomach cancer:
Here are a few steps you can take to minimise the risk:
- High intake of fruits & vegetables, especially those with antioxidants (B carotene, vitamin C, E, and folate)
- Reduce intake of sodium/salt, preserved or pickled foods, red meat, cured meat
- Reduce alcohol intake
- Reduce or quit smoking
- Regular endoscopic screening every 2-3 years
- Helicobacter Pylori elimination
Summary
Stomach cancer, while not entirely preventable, has a number of known risk factors which can be easily reduced by adopting healthy lifestyle choices and attending routine screenings. If you experience any of the symptoms mentioned above, please contact us at Alpha Digestive Liver Centre. We will arrange a consultation for you with our gastroenterologist, Dr. Benjamin Yip, for a proper diagnosis and personalised treatment plan.
References
- “Case-control study of diet and other risk factors for gastric cancer in Hawaii (United States).” PubMed, https://pubmed.ncbi.nlm.nih.gov/12948286/. Accessed 6 October 2022.
- “Gastric cancer: epidemiology, prevention, classification, and treatment.” NCBI, 7 February 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5808709/. Accessed 6 October 2022.
- “Stomach Cancer.” Singapore Cancer Society, https://www.singaporecancersociety.org.sg/learn-about-cancer/types-of-cancer/stomach-cancer.html. Accessed 6 October 2022.
- “Stomach Cancer — Cancer Stat Facts.” Surveillance, Epidemiology, and End Results Program, https://seer.cancer.gov/statfacts/html/stomach.html. Accessed 6 October 2022.
- “Stomach cancer in young people – a diagnostic and therapeutic problem.” NCBI, 20 December 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6983757/. Accessed 6 October 2022.

