Gastritis and duodenitis are conditions where the lining of the gastrointestinal tract becomes inflamed. The key difference to note is the location of the inflammation. Gastritis affects the stomach lining, while duodenitis involves the inflammation of the first part of the small intestine (duodenum). Both of these conditions can affect men and women of all ages and can be chronic or acute. This article will help you better understand how these two conditions can be effectively managed by delving into their causes, symptoms, and treatment options.
Symptoms and Common Causes of Gastritis and Duodenitis
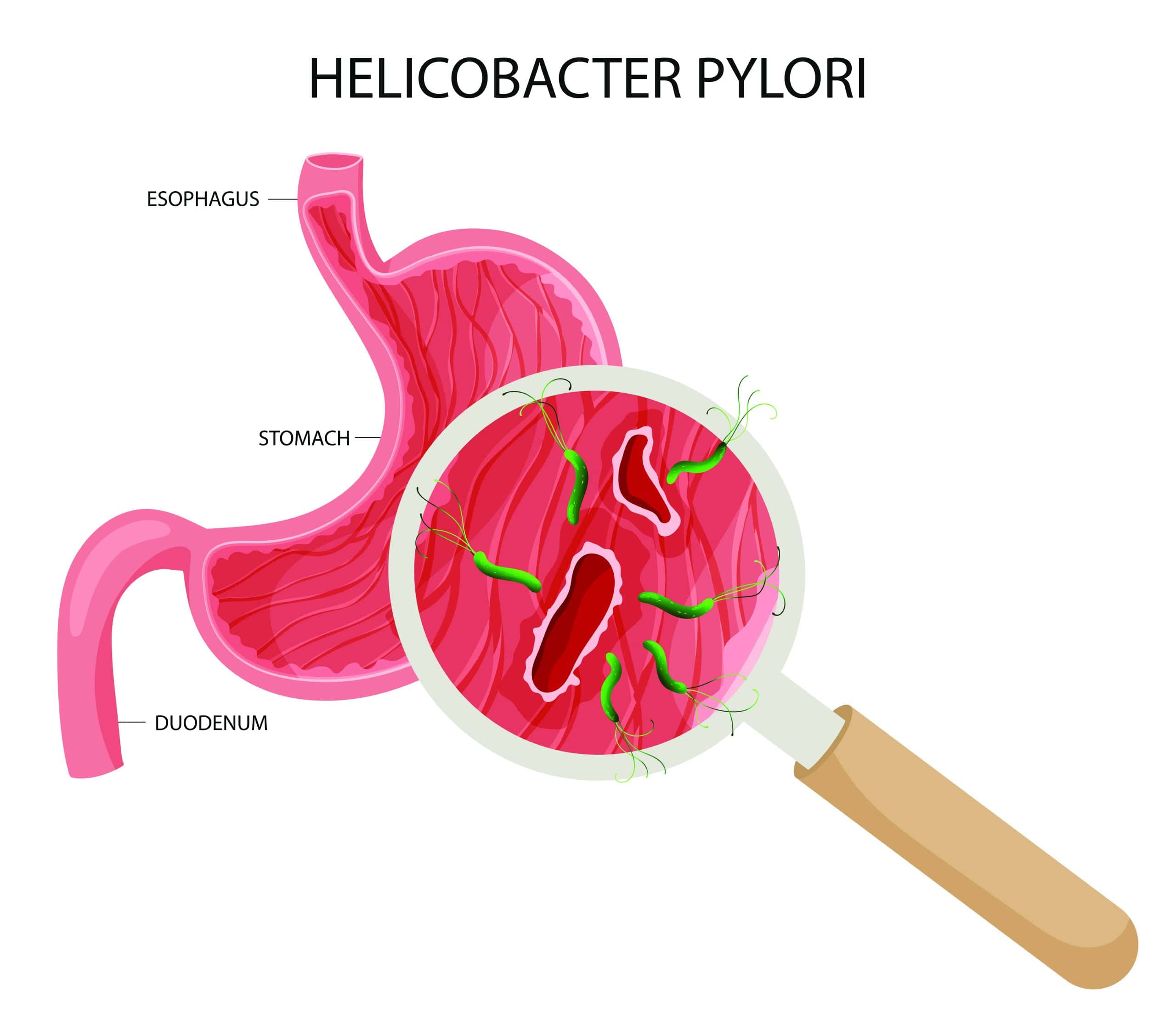
The most common cause of gastritis and duodenitis is infection through a bacterium known as Helicobacter pylori, which can irritate the mucus lining and cause inflammation. H. pylori can be transferred from one individual to another and can come from various sources, such as contaminated food and water.
The other duodenitis and gastritis causes are:
- The use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as Ibuprofen and Aspirin.
- Excessive alcohol consumption
- Stress
- Cigarette smoking
- Certain auto-immune diseases, such as Crohn’s disease
Gastritis and duodenitis often share similar symptoms due to their similar impact on the digestive system. Common duodenitis and gastritis symptoms can include:
- Loss of appetite: Reduced desire to eat due to discomfort and feeling full soon after eating.
- Abdominal pain: A burning or gnawing pain in the upper abdomen, which may feel worse on an empty stomach.
- Indigestion or heartburn: A burning sensation in the chest or stomach, especially after eating.
- Nausea and vomiting: A frequent sensation of nausea and sometimes vomiting.
- Bloating and gas: A feeling of fullness in the stomach and increased gas production.
- Belching: Increased burping, which may help relieve gas and bloating.
- Black, tarry stools: This may indicate bleeding in the stomach or duodenum and should be reported to a doctor.
- Fatigue: In some cases, due to issues with nutrient absorption.
Diagnosis and Treatment
Gastritis and duodenitis are diagnosed through a combination of medical history, physical examination, and diagnostic tests. A Gastroenterologist will ask you about symptoms such as abdominal pain, nausea, and indigestion, as well as any potential causes, like the use of NSAIDs or alcohol consumption. A physical examination and various tests may also be conducted to diagnose the condition and subsequently recommend relevant treatment. These can include:
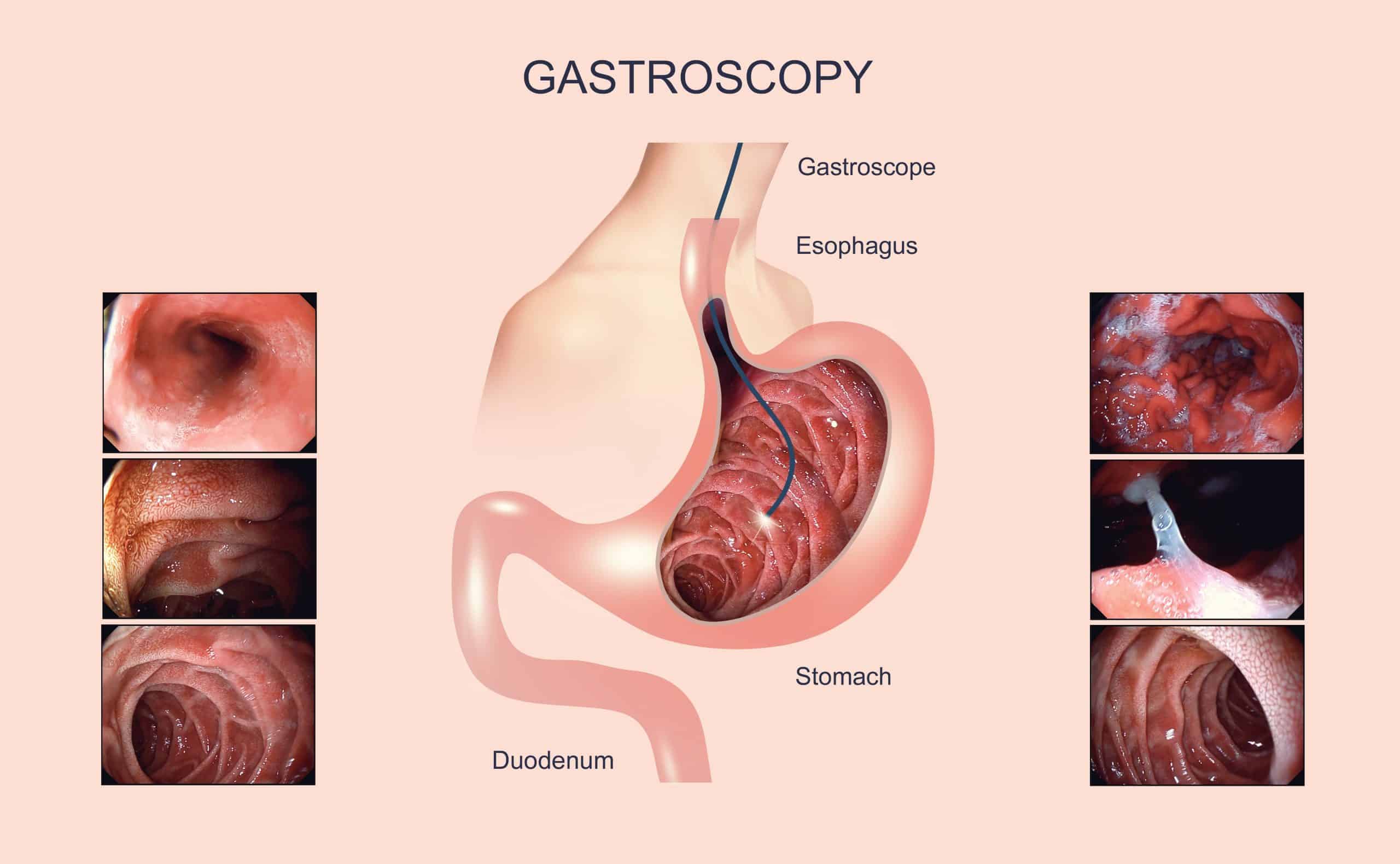
- Gastroscopy: A Gastroscopy involves inserting a flexible, thin tube down a person’s throat into the stomach with a camera attached to the end. Often, doctors use this procedure to confirm a diagnosis and collect tissue samples, if necessary.
- H. Pylori breath test: Commonly known as a urea breath test, this is a non-invasive diagnostic method for H. pylori infection. The patient drinks a urea solution, and if H. pylori is present, it will break down the urea into carbon dioxide, which is detectable in the breath.
- Blood test: Blood tests can be used to check for anaemia (a potential side effect of chronic gastritis) and the presence of antibodies to H. pylori.
- Stool test: This will check for H. pylori antigens in the stool, which can help diagnose an infection.
Gastritis and duodenitis are generally curable with appropriate treatment. Effective treatment for gastritis and duodenitis varies from person to person, depending on the underlying causes and the individual's stringent adherence to the advised treatment plan.
If an H. pylori infection is found to be the cause, your doctor may recommend triple therapy treatment. This encompasses a simple medication regime of one proton pump inhibitor (PPIs work by blocking the cells that produce acid in the stomach) with two antibiotics, taken for 14 days as advised by your doctor or medical professional.
Furthermore, depending on the causes and severity of the disease, alternative duodenitis and gastritis treatment may be recommended. This could include making certain lifestyle changes, such as reducing or stopping NSAIDs, or limiting alcohol and tobacco intake. If a doctor finds that an individual is gluten-intolerant, or has celiac disease, he/she will need to remove gluten from their diet to avoid an inflammatory flare-up.
Complications
If poorly controlled or left untreated, gastritis or duodenitis can result in serious complications such as bleeding of the lining/mucosa of the gastrointestinal tract, fever, and peptic ulcer disease, which may increase the risk of stomach or duodenal cancer. Long-term damage can also result in scarring, strictures, or obstruction in the digestive tract.
What Are the Other Conditions That Can Present Similar Symptoms
Several other conditions can present symptoms similar to those of gastritis or duodenitis, including peptic ulcer disease, gastroesophageal reflux disease (GERD), celiac disease, irritable bowel syndrome (IBS), Crohn's disease, and ulcerative colitis. Additionally, gallbladder disease, pancreatitis, and certain infections or malignancies in the gastrointestinal tract can also cause similar symptoms, such as abdominal pain, nausea, vomiting, and bloating. It's important to seek medical evaluation for a proper diagnosis if you experience persistent or severe symptoms to rule out other underlying conditions and receive appropriate treatment.
When to Seek Medical Attention from a Gastroenterologist
Consult a Gastroenterologist if you experience persistent or severe symptoms of gastritis or duodenitis, such as intense abdominal pain, nausea, vomiting (especially if it's bloody), loss of appetite, unexplained weight loss, difficulty swallowing, or black, tarry stools. Additionally, if over-the-counter treatments and lifestyle changes do not alleviate your symptoms, consult a specialist for further evaluation and appropriate treatment.
Preventative Tips
Preventing gastritis and duodenitis involves making lifestyle changes that help protect the stomach and duodenal lining from irritation and inflammation. Here are some preventative measures:
- Consume a healthy diet: Avoid spicy, acidic, or greasy foods that may irritate the stomach lining. Instead, focus on a balanced diet rich in fruits, vegetables, and whole grains.
- Eat smaller meals: Eating smaller, more frequent meals can help reduce pressure on the stomach and prevent irritation.
- Limit alcohol and caffeine: Excessive consumption of alcohol and caffeinated drinks can increase the risk of gastritis and duodenitis. Limit the intake of these drinks or avoid them altogether.
- Avoid NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and aspirin can cause stomach irritation. Use them sparingly and only as directed.
- Quit smoking: Smoking irritates the stomach lining and can increase the risk of gastritis.
- Manage underlying conditions: If you have other medical conditions, such as autoimmune disorders, treat them under the supervision of a qualified physician.
Summary
If you're experiencing gastritis or duodenitis, it's crucial to seek medical advice for an accurate diagnosis and treatment plan tailored to your condition. Additionally, regular follow-ups with your Gastroenterologist are essential to monitor progress and adjust treatment as needed for optimal management of gastritis or duodenitis.
For tailored specialised advice from Dr Benjamin Yip, the Medical Director of Alpha Digestive & Liver Centre and an experienced Consultant Gastroenterologist, please book an appointment with us.
Frequently Asked Questions
What causes gastritis?
Several factors, including infection with H. pylori bacteria, long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin, excessive alcohol consumption, smoking, stress, and certain medical conditions like autoimmune disorders, can cause gastritis.
What are suitable treatments for gastritis?
Treatment for gastritis often depends on the diagnosis/underlying causes. Doctors may prescribe antibiotics along with PPI medications for H. pylori infection. For H. pylori infection, antibiotics may be prescribed along with PPI medications. If NSAIDs or alcohol are the causes, stopping or reducing their use can help.
Can gastritis go away on its own?
Sometimes, addressing the underlying cause can resolve gastritis on its own. For instance, if the use of NSAIDs or alcohol consumption causes gastritis, stopping these substances can aid in improving the condition. However, medical treatment may be required for more severe or chronic cases of gastritis, as well as for long-term relief. In these cases, it is advisable to seek specialised care from a Gastroenterologist.
How do you relieve gastritis?
Besides receiving treatment from a Gastroenterologist, you can make lifestyle adjustments as well. This could include avoiding spicy, acidic or greasy foods that irritate the stomach, eating smaller meals, limiting alcohol and caffeine, and managing stress with relaxation techniques such as meditation, deep breathing, or yoga, as stress can contribute to stomach irritation. Over-the-counter medications may also provide immediate relief from pain, but they may not be a permanent solution.
For more insights on Gastroscopy and Colonoscopy, check out this interview with Dr Benjamin Yip, Gastroenterologist in Singapore.
References
- Kivi, Rose. “Gastritis/ Duodenitis”, Healthline, July 24 2020, https://www.healthline.com/health/gastritis-duodenitis#gastritis-duodenitis-and-ibd
- Robertson, Sally. “Gastritis Diagnosis”, News Medical, 15 June 2023, https://www.news-medical.net/health/Gastritis-Diagnosis.aspx
- Davis, Charles Patrick. “Gastritis”, MedecineNet, 12 August 2023, https://www.medicinenet.com/gastritis/article.htm

